Achieving Closure: Factors That Lead to Wound Healing
April 30, 2020
By the WoundSource Editors Wound healing is a highly complex chain of events that allows the skin to repair and regenerate to provide protective functions, such as temperature modulation, and moisture regulation, as well as sensation reception and transmission.1 Although very complex processes occur if a wound is going to heal, we generally recognize four phases that wounds progress through to achieve complete closure2:
- Homeostatic phase: Platelets aggregate, and clotting factors form a fibrin clot to create a protective layer over the wound.
- Inflammatory phase: The wound swells as damaged cells, pathogens, and bacteria are removed.
- Proliferative phase: Granulation occurs, and new tissue is rebuilt within the wound.
- Remodeling phase: The wound is fully closed, but collagen fibers are rearranged through cross-linking to improve tensile strength and reduce the scar’s appearance.
For this process to occur successfully, certain molecular requirements must be met. Poor oxygenation is a recognized cause of delayed healing. Oxygen is central to many levels of wound healing, including collagen synthesis. Nutrition, including the availability of proper protein stores and specific vitamins and minerals— such as vitamin C, vitamin A, and zinc, is also crucial. These nutrients are necessary for the process of cross-linking, reducing oxidative stress, reducing susceptibility to wound infection, and for proper DNA and RNA synthesis.1
Debridement
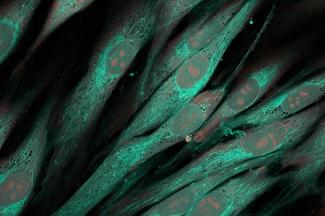
These molecular requirements can often be negatively impacted by the presence of necrotic or non-viable tissue. The delivery mechanisms for oxygen and nutrients are interrupted. Debridement may be deemed a necessary intervention for converting a chronic wound to an active, healing wound. When the necrotic tissue is removed, the wound can be returned to an acute status, and the healing process can move forward. There are several specific ways in which debridement promotes the healthy progression of wounds through the healing process. During the inflammatory phase of healing, neutrophils provide interleukin, which is a stimulus for the proliferation of keratinocytes.1 Keratinocytes are integral to the entire wound healing process and are involved in the initiation, maintenance, and completion of wound healing.3 Keratinocytes within non-healing wounds and at their healing edges are often different from normal, healthy keratinocytes. Yet, the healthy communication that occurs between healthy keratinocytes and other cell types, including fibroblasts, is integral to healing and essential for successful wound closure. Keratinocytes recruit, stimulate, and coordinate the actions of multiple cell types that are crucial in the healing process.4 The proliferative phase of healing is marked by the presence of processes such as angiogenesis, extracellular matrix formation, and epithelialization. Platelet-derived growth factor can promote proteoglycan and collagen formation. The local fibroblasts respond to platelet-derived growth factor by producing collagen and transforming into myofibroblasts, which cause the wound to contract.5 The foundation for the biological argument for debridement is related to these processes. By removing the unhealthy cells from the wound edge and exposing them to healthy cells with high regenerative potential, epithelialization and healing of chronic wounds are enhanced.3 When this necrotic tissue is removed, the wound can access and utilize the regenerative potential of surrounding, healthy tissue. For this reason, preservation of the bordering viable tissue is crucial, especially when there is limited adjacent tissue. After the non-viable tissue has been removed, the wound can transition to a granulating wound. These strategies work to support the complex processes throughout the four stages of healing to achieve closure more successfully.
References 1. Childs DR, Murphy AS. Overview of wound healing and management. Surg Clin North Am. 2017;97:189-207. 2. What are the stages of wound healing? Advanced Tissue. 2018. https://advancedtissue.com/2018/11/what-are-the-stages-of-wound-healing/. Accessed March 27, 2020. 3. Pastar I, Stojadinovic O, Tomic-Canic M. The role of keratinocytes in healing chronic wounds. Surg Technol Int. 2008;17:105-112. 4. Wojtowict AM, Oliveira S, Carlson MW, Zawadzka A, Rousseau CF, Baksh D. The importance of both fibroblasts and keratinocytes in a bilayered living cellular construct used in wound healing. Wound Repair Regen. 2014;22(2):246-255. 5. Reinke JM, Sorg H. Wound repair and regeneration. Eur Surg Res. 2012;49:35-43.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.








Follow WoundSource
Tweets by WoundSource