Chronic Fungal Skin Infection Treatment and Prevention
September 29, 2016
It doesn't matter where exactly I am educating, I see it everywhere: the vicious cycle of chronic intertrigo and/or candida infections (candidiasis) of the skin in the long-term care arena. Skin and soft tissue infections are the third most common infection in long-term care.
This ongoing problem is now receiving more attention due to state surveyors becoming certified in wound care. State surveyors will be up-to-date on skin and wound care management. Law firms are also advertising any type of skin breakdown as a negligence issue. Moisture-associated skin damage (MASD) and fungal skin infections are preventable. Fungal skin infections that lead to further skin breakdown equal poor quality of care.
I observe health care provider orders time and time again for antifungal powders/creams, numerous types of ointment/creams, and even nurses whipping up their own concoctions to treat fungal infections of the skin. Nurses should protect their license and remember that compounding is the pharmacist's job. I have also observed antifungal treatment orders in place for up to two years! Why? Recurring fungal rash/infections, due to gaps in nursing education. We as wound care clinicians must help to close these gaps.
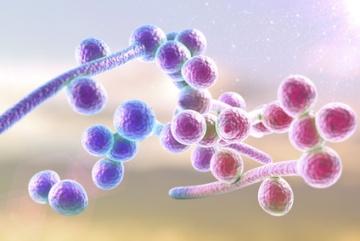
Intertrigo and Yeast or Candida Skin Infections
Intertrigo is caused by moisture being trapped in skin folds. A dark warm area along with skin on skin friction will harbor bacteria, fungus and yeast. The symptoms typically include odor, itching and burning. Commonly affected areas include under the breasts, skin folds on the belly or thighs, the armpits and groin. However, it can happen anywhere there is moisture against the skin with a lack of air circulation.
Most people suffer from yeast (candida) skin infections in the perineal, buttock, and groin area. Some of the common symptoms of yeast infection are red, pimple-like bumps, with severe itchiness.
Skin Care 101: How to Prevent Fungal Skin Infections
- Cleanse skin with a pH balanced skin cleanser, no-rinse cleanser, or mild soap/water, then rinse.
- Dry the skin thoroughly. Soft cloth or pat dry technique.
- Incontinence care: Apply a skin sealant or barrier cream containing zinc oxide. All steps must be repeated after each incontinence episode. (Follow your policy and procedures for incontinence care. Check and change every 2 hours, etc.)
- Other locations: Moisturize with lotions containing lanolin or a petrolatum base. This will serve as a protective barrier.
Nurses and nursing assistants should be provided with ongoing skin care regimen education. While it may seem to be a simple skill or task, skin care regimen steps are not followed through on. So how can we help? When I go inside facilities, I recommend the Wound Nurse, Charge Nurse, or Unit Manager follow all nursing staff periodically to check skills with skin care, brief changing, and offloading techniques. Nurses must apply creams and ointments that cannot be kept at the bedside. This also shows monitoring of the affected skin sites. Prevention measures should be in place for fungal skin infections, especially for the obese patient. Bed linens, paper towels, or dressings should not be used to separate skin folds. There are many moisture-wicking fabrics impregnated with antimicrobial properties available for skin moisture management.
References:
Black JM, Gray M, Bliss DZ, et al. MASD part 2: incontinence-associated dermatitis and intertriginous dermatitis: a consensus. J Wound Ostomy Continence Nurs. 2011 Jul-Aug;38(4):359-70; quiz 371-2.
Gould D. Diagnosis, prevention and treatment of fungal infections. Nurs Stand. 2011 Apr 20-26;25(33):38-47; quiz 48.
Lowe JR. Skin Integrity in Critically Ill Obese Patients. Crit Care Nurs Clin North Am. 2009 Sep;21(3):311–v.
Mouton CP, Bazaldua OV, Pierce B, Espino DV. Common infections in older adults. Am Fam Physician. 2001 Jan 15;63(2):257-68.
About the Author
Cheryl Carver is an independent wound educator and consultant. Carver's experience includes over a decade of hospital wound care and hyperbaric medicine. Carver single-handedly developed a comprehensive educational training manual for onboarding physicians and is the star of disease-specific educational video sessions accessible to employee providers and colleagues. Carver educates onboarding providers, in addition to bedside nurses in the numerous nursing homes across the country. Carver serves as a wound care certification committee member for the National Alliance of Wound Care and Ostomy, and is a board member of the Undersea Hyperbaric Medical Society Mid-West Chapter.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











Follow WoundSource
Tweets by WoundSource