How Can You Prevent Medical Adhesive-Related Skin Injuries?
March 4, 2021
Introduction
“Top-down skin injuries” is an increasingly common term used to describe superficial cutaneous injuries. Top-down injuries result from damage beginning at the skin’s surface or the soft tissue. In contrast, “bottom-up injuries” are often the result of ischemia. Top-down injuries usually result from mechanical forces, inflammation, or moisture. Common top-down injuries are moisture-associated skin damage, skin tears, and medical adhesive–related skin injury (MARSI). In this blog, I focus on assessing, defining, and preventing MARSI.1
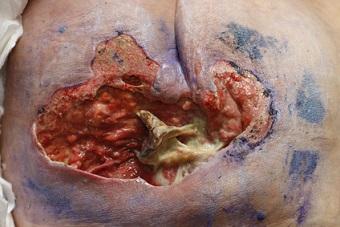
MARSI is a term that was developed to describe and define a clinical problem. MARSI is defined as erythema, vesicles, erosion, tears, or bullae persisting 30 minutes or more after removal of an adhesive dressing.1 Adhesive use is common in health care settings. Adhesives are used to secure dressings, medical devices, and equipment. Additionally, many medical devices have an adhesive that is used to adhere to the patient (ostomy pouches, condom catheters, catheter securement devices, electrodes, and surgical drapes). The barrier function of these medical devices is highly dependent on the integrity of the stratum corneum. A break in the skin integrity of the stratum corneum causes a risk for compromise in the skin barriers discussed earlier.1
Who Is at Risk?
Age is definitely a significant risk factor for MARSI (read my previous blog, Geriatric Skin Changes: What's Normal and What's Not?).2 Skin maturation is also a risk factor, in infants and children. Dehydration, poor nutrition, impaired sensory perception, impaired thermoregulation, increased fall risk, use of soaps, impaired mobility and dry skin are also significant risk factors for MARSI. Intrinsic and extrinsic risk factors can be broken down as follows:
Intrinsic
- Older adults and infants (skin changes related to aging)
- Epidermal thinning, decreased collagen, subcutaneous tissue loss, and reduced elasticity of skin
- Dehydration
- Poor nutrition
- Impaired mobility
- Impaired sensory perception
- Change in mental status
- Specific to neonates: deficient stratum corneum and impaired thermoregulation
Extrinsic
- Risk of mechanical trauma (during activities of daily living or transfers)
- Use of soap or type of soap used
- Dry skin (increased risk for friction and shear)
- Impaired mobility (cannot reposition independently)
- Sharp corners or edges on wheelchair, bed, table, etc., that are not padded1
There isn’t actually a risk assessment scale specific to MARSI, but if the categories of the Braden Scale for Predicting Pressure Sore Risk® are broken down, you will see that many of the same risk factors for pressure injuries apply to MARSI. Additionally, MARSI is almost always a preventable skin issue.
Speaking of Prevention… How Can We Best Prevent MARSI?
The first step to prevent is to identify the cause or setting. MARSI manifests differently in different settings (think long-term care, intensive care, the operating room, medical surgical areas… different levels of care). First, we need to assess the care setting, our patient, and the risk factors for MARSI (discussed earlier). Choosing the correct adhesive products for the patient is critical. Different tapes or nylon adhesives may damage the integrity of fragile skin. The skin should be prepared before applying the adhesive product (shaving as needed, using liquid barrier film).
The adhesive product must be properly applied and removed (technique).Inappropriate removal of adhesives is a frequent cause of MARSI. Adhesives should be removed at a horizontal angle (low), and the skin adjacent to the peel line should be supported during removal to prevent pulling, irritation, and MARSI.1 The clinician should also be knowledgeable about adhesive selection and adhesion level, along with the ingredients of the backing or adhesive, and what level of adhesion they apply.
The level of adhesion needed to secure the dressing or device should also be examined here. Silicone adhesives are typically gentler adhesives, whereas polyester or silk adhesives typically provide a higher level of adhesion. A cloth and paper combination provides a moderate level of adhesion. Risk for mechanical injury, current integrity of the skin, microclimate, and elasticity should all be assessed before selecting and applying an adhesive product. Selecting the correct adhesive involves a thorough skin assessment of each patient and is definitely individualized. Patch testing can also be done before checking for any reaction, especially when applying adhesive to a larger surface area. Adhesive alternatives should also be explored for patients with sensitive skin or an adhesive sensitivity. Tubular elastic dressing, netting, or conforming bandages are options. An abdominal binder may also be considered, depending on what needs to be secured. Staff education on prevention is important. Initial and ongoing education on new products, prevention, and treatment is a critical part of a strong skin prevention and treatment program.
Note
Keep an eye out for future blogs on specific adhesive alternatives and treatment of MARSI.
References
1. Thayer D, Rozenboom B, & Baranoski S. “Top-down” injuries: prevention and management of moisture-associated skin damage (MASD), medical adhesive-related skin injury (MARSI), and skin tears. In: Doughty DB, McNichol LL, eds. WOCN Society Core Curriculum: Wound Management. Philadelphia, PA: Wolters Kluwer; 2016:281-312.
2. Hovan H. Geriatric skin changes: what’s normal and what’s not. WoundSource.com. 2018. https://www.woundsource.com/blog/geriatric-skin-changes-what-s-normal-a…. Accessed January 20, 2021.
About the Author
Holly is a board-certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











Follow WoundSource
Tweets by WoundSource