Is it Moisture-Associated Skin Damage or a Pressure Ulcer?
April 28, 2015
Being an independent wound care education consultant in long-term care, I get a lot of questions regarding moisture-associated skin damage (MASD). Is it MASD or a pressure ulcer? When do I change it from MASD to pressure ulcer in my documentation? I also observe documentation stating, "skin excoriation" when referring to MASD. This term is often used incorrectly. Excoriation is linear erosion due to mechanical means. "Denuded" is the correct term when describing the loss of epidermis, caused by prolonged moisture and friction. My goal in writing this blog, is that it will help those clinicians that struggle with identifying, and managing MASD, specifically for incontinence-associated dermatitis (IAD).
What is MASD?
MASD is inflammation and erosion of the skin caused by prolonged exposure to various sources of moisture, including urine/stool, perspiration, exudate, ostomy effluent, mucus, and saliva. MASD is based on chemical content of moisture, friction, and presence pathogenic organisms. The injury starts at the top layer of the skin, and works inward leading to partial thickness. The tissue is pink or red in color. There can be other attributes as the aging process, medication changes, hormone imbalances, infections, and dementia. However, these attributes should not be excused as a consequence of a condition associated with advanced age. MASD is divided into four categories:
Incontinence-Associated Dermatitis (IAD): Inflammation and skin erosion associated with exposure to urine and or stool.
Intertriginous Dermatitis: Intertrigo is the inflammation in skin to skin, or skin to device related to perspiration, friction, bacterial, and or fungal bioburden.
Periwound Moisture-Associated Dermatitis: Wound exudate that has sustained contact with the skin causing damage. Inflammation and erythema to skin with or without erosion.
Peristomal Moisture-Associated Dermatitis: Inflammation surrounding a stoma due to sustained contact of stool or urine. In long-term care, IAD is a particular challenge for clinicians as many clients are at increased risk due to issues of incontinence, age and other health conditions. Following are primary factors that increase the risk of developing IAD:
- Tissue tolerance - age, health, nutrition, oxygen level/perfusion, and core body temperature.
- Perineal environment - Type of incontinence, irritants, enzymes, skin pH, and fungus/bacteria.
- Toileting ability - Mobility, sensory perception, cognitive awareness, occlusive containment products.
- Mechanical trauma/chafing/friction - Aggressive skin cleansing, absorbent pads/briefs, occlusive containment products.
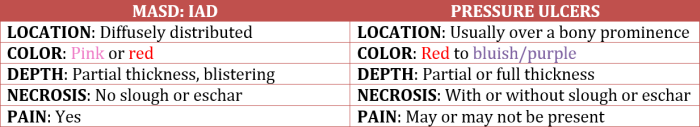
When is it MASD and When is it Pressure?
Regular inspection of the skin is essential in identifying damage resulting from moisture and/or pressure. The following chart provides a basic guidelines for distinguishing IAD from the formation of pressure ulcers:
Prevention of Incontinence-Associated Dermatitis
Preventing IAD will help decrease the cost of care, improve quality of life, decrease suffering, and prevent pressure ulcer development.
- Cleanse skin gently after every incontinence episode, using a pH no-rinse skin cleanser. Cleansers actually lessen the cleansing time than traditional cleansing with soap and water. Many cleansers already contain a variety of additives, simplifying the cleansing process. Ex: antiseptics, emollients, humectants, and moisturizers.
- Moisturize dry skin to maximize lipid barriers. Moisturize at minimum twice daily.
- Protect with a moisture barrier as indicated. Most common skin barriers used are petrolatum (if urine only), otherwise dimethicone and zinc oxide.
Skin Management
Ongoing education is key in establishing an effective skin management program. IAD and other forms of MASD are preventable and manageable. Management of incontinence is an indicator of quality of care in the long-term care arena. It can impact your facility reimbursement and five star rating score. Document MASD according to your facility's protocol.
About the Author
Cheryl Carver is an independent wound educator and consultant. Carver's experience includes over a decade of hospital wound care and hyperbaric medicine. Carver single-handedly developed a comprehensive educational training manual for onboarding physicians and is the star of disease-specific educational video sessions accessible to employee providers and colleagues. Carver educates onboarding providers, in addition to bedside nurses in the numerous nursing homes across the country. Carver serves as a wound care certification committee member for the National Alliance of Wound Care and Ostomy, and is a board member of the Undersea Hyperbaric Medical Society Mid-West Chapter.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











Follow WoundSource
Tweets by WoundSource