Lower Extremity Arterial Disease (LEAD) Awareness and Discussion
September 22, 2021
Peripheral artery disease (PAD) is also known as lower extremity arterial disease (LEAD), peripheral arterial occlusive disease (PAOD), or arteriosclerosis obliterans.1 LEAD is a disease that impacts the circulatory system, specifically the arteries (narrowing, which can result in a decreased supply of blood flow to the limb), and can eventually lead to limb loss or amputations. It is important to bring awareness to LEAD and its diagnosis, treatment, and prevention to improve access to care and screenings and ultimately to prevent limb loss. LEAD may be unrecognized and at times an underdiagnosed manifestation of atherosclerosis.
The presence of LEAD is often defined by an ankle brachial index (ABI) of 0.90 or less. It is estimated that LEAD affects 8.5 million Americans ages 40 and older and, globally, 202 million adults. Older adults are at a higher risk for a diagnosis of LEAD.1
Pathophysiology of LEAD
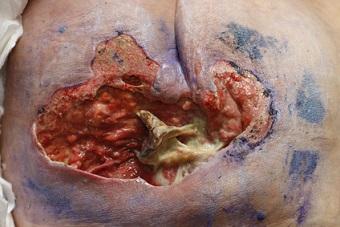
LEAD is a chronic and progressive disease that is often caused by atherosclerosis or fatty deposits in the arteries. As atherosclerosis progresses, artery walls become rigid, preventing dilation in response to tissue demands for blood flow and oxygen. Clinically, this is seen as progressive pain with walking that is relieved by rest (claudication). Advanced disease may result in ischemic wounds related to impaired tissue perfusion.1 Systemic support and appropriate topical therapy are essential to promote healing and maintain skin integrity. Identifying and treating infection, removing necrotic tissue (if not contraindicated by perfusion status), protecting the wound surface from pressure, and managing exudate while maintaining a moist wound environment are included in this approach. Interventions are tailored to the specific need of the patient or wound, and ABI interpretation is one tool to help guide the wound management plan.1
Common Risk Factors
- Obesity*
- Smoking*
- High blood pressure*
- High cholesterol*
- Increased age
- Family history
The risk factors followed by an asterisk (*) are elements that may be modified with lifestyle changes. Unfortunately, age and family history are unmodifiable risk factors. A common recommendation for LEAD prevention and treatment is aggressive risk factor modification; for example, weight loss, stopping or decreasing smoking, diet control (for blood pressure and cholesterol), and exercise. Education is a huge part of prevention, along with follow-up and ensuring or promoting accessible care.
Signs and Symptoms
- No symptoms
- Leg pain when walking that improves at rest (claudication); calf pain is common
- Cooler skin temperature
- Hair loss on the extremity
- Shiny skin on the extremity
- Weak or absent pulses
- Cramping, numbness, or weakness in the extremity
Ischemia can impact nerve function in the extremities; therefore, patients with LEAD should be screened for neuropathy.1 Hallmark signs of an acute limb threat (e.g., occlusion) are sudden onset of the six Ps: pulselessness, pain, pallor, paresthesia, paralysis, and polar (cold).1
Conclusion
Ideally, our goal is primary prevention, but if that is not possible, secondary prevention and treatment are next. Education is a huge concept when it comes to a successful treatment plan for patients with LEAD. These are just some small tidbits and tips of the iceberg when it comes to LEAD; awareness and prevention are essential and are two of the concepts we focus on in September, PAD awareness month!
Reference
1. Bonham P. Assessment and management of patients with wounds due to lower extremity arterial disease (LEAD). In: McNichol LL, Ratliff CR, Yates SS, eds. Wound, Ostomy and Continence Nurses Society Core Curriculum: Wound Management. 2nd ed. Philadelphia, PA: Wolters Kluwer; 2022:493-538.
About the Author
Holly is a board certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











Follow WoundSource
Tweets by WoundSource