Surgical Wound Management and Ostomy Education: An Interdisciplinary Approach to Abdominoperineal Resection (APR)
August 5, 2020
An abdominoperineal resection (APR) is an operation in which a surgeon removes the anus, rectum, and sigmoid colon, usually to treat low rectal cancers. Pre-procedure, the patient should be educated on the procedure, how it is done, what to expect post-operatively (immediately and long term), and ostomy education. Because the anus and rectum are removed during surgery, a permanent colostomy is created. It is important for the patient to understand that the perineum will be sewn closed during the operation, and they will wake up with an ostomy pouch in place. The patient should be marked for their colostomy before surgery by a trained and certified ostomy specialist, to ensure optimal outcomes related to independence with ostomy care and stoma placement.
The colostomy created during an APR procedure is typically located on the left side of the abdomen, given abdominal anatomy, but it could be on right side depending on operative findings. (Please see my earlier blog on the importance of pre-operative stoma site marking for details.)
Tips and Tricks for People with New Ostomies: Adjusting to Life After Surgery
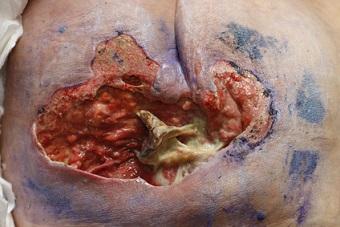
Post-surgery, the patient will have an ostomy, a perineal wound, and abdominal surgical incisions (the size and number of incisions depend on the type of procedure, open vs. closed, complications, etc.). The patient will recover in the hospital for a period of time before returning home or for rehabilitation.
Issues Related to Wound Care
In the pre- and post-operative periods, and while the patient is recovering, it is important that there is management by an interdisciplinary team. The team includes the following: the surgeon; the primary care provider; a dietitian; physical and occupational therapists; a wound, ostomy, continence (WOC) nurse specialist; and other specialty providers, depending on the patient's needs and medical diagnosis (hematology or oncology if there is a cancer diagnosis). Having a dietitian to discuss an ostomy diet, along with the importance of nutritional intake as this relates to wound healing, is important.
Collaborating with physical and occupational therapists is critical in formulating an individualized therapy plan and a seating assessment, given the new perineal surgical wound. Preventing wound dehiscence and complications is important, especially in the immediate post-operative period. A WOC nurse specialist is also an important player in the post-operative period, both while the patient is in the hospital and post-discharge at home.
The WOC nurse serves as the patient’s support system related to WOC needs (ostomy management and perineal and abdominal wounds). The WOC nurse helps the patient to transition back to a new normal and to understand and complete ostomy care independently (or with the help of a caregiver) and wound healing and complications. Understanding lifestyle modifications and changes, travel-related issues, and body image are important topics that the WOC nurse specialist should address. It is helpful to provide both verbal and written instruction and to watch the patient demonstrate ostomy care independently using the teachback method.
Some important key points to keep in mind post-operatively are:
- Ostomy management: Enable independence and provide support.
- Be sure that an appropriate seating surface is in use, and encourage side sleeping, as well as sitting for short intervals initially.
- Be mindful with lifting, pushing, pulling, and other activities: Specific guidance from the surgeon related to what can and cannot be done in the post-operative period, and how to advance with exercise and movement, should be included in the plan of care.
Conclusion
As mentioned earlier, taking an interdisciplinary approach to patient management with this complex surgery is imperative for the best outcomes. Each member of the team contributes to a successful pre- and post-operative course. Allowing time for the patient to ask questions and providing instruction and hands-on demonstration when needed are important. Having support and a support system beyond immediate family in the post-operative period is also important. APR surgery is life-changing and lifesaving in many ways; when a patient feels supported and has the knowledge and skill to manage their care (with help as able), the return to a new normal lifestyle is an easier transition.
About the Author
Holly is a board-certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











Follow WoundSource
Tweets by WoundSource