Washing Our Hands of Healthcare-Acquired Infections
May 8, 2014
Part 5 in a series on infection management
Part 1 | Part 2 | Part 3 | Part 4
By Bruce E. Ruben MD
According to the American Hospital Association, over 36 million patients are admitted to hospitals every year. Presumably, these patients go to hospitals to get well, but one in 20 end up getting something else: an infection. Worse, one in nine of those infections result in death.
The statistics vary among reporting agencies including the Centers for Disease Control and Prevention (CDC), the Department of Health and Human Services and the Centers for Medicare & Medicaid services. But, the situation is bleak no matter whose report you’re reading.
The numbers are startling just by themselves. But when you consider how these infections are acquired, they become tragic. For example, a patient goes into the hospital for a routine appendectomy and ends up dying from Clostridium difficile (C-diff) related colitis, an antibiotic-resistant bacteria that originated in some other patient’s colon.
How Multidrug-Resistant Bacteria Colonize and Travel
How did the bacteria travel inside the hospital to infect the appendectomy patient? It’s simple. Bacteria can travel by any hospital care worker making direct patient contact or making contact with the myriad of devices inserted in patients, including, most often, venous catheters and urinary catheters.
Maybe it was the nurse who wasn't diligent enough with her hand washing. Perhaps it was the physician who touched a contaminated surface right before rounding. Somehow, though, feces went from point ‘a’ to point ‘b’ without adequate intervention.
Almost 100,000 patients a year acquire an infection from something as ubiquitous and seemingly innocuous as a urinary catheter. How? It could be the catheter was left in too long, thus keeping the entire urinary tract vulnerable to infection from inside the body and outside. Maybe the catheter was installed under less than ideal aseptic conditions.
Here, two points need to be made. First, there are many avenues within the hospital setting where multidrug-resistant and deadly bacteria can travel, colonize and invade. Of course, hospitalized patients are the most vulnerable due to their underlying medical problem in the first place. That’s the nature of the hospital beast and really, it applies to any inpatient healthcare setting.
Most importantly, hospital strains of bacteria are exposed to the broadest and most expansive spectrum antibiotics that have easily mutated to resist those drugs. With the exception of Methacillin Resistant Staph Aureus (MRSA), most of the remaining multidrug-resistant bacteria remain within hospitals and other inpatient facilities. Still, some patients have already experienced the end of the antibiotic rope.
4 Ways to Prevent the Spread of Healthcare-Acquired Infections
That’s why we all need to evaluate the social causations of this problem. That is the social conditioning that considers hospitals as the first choice, safe haven model to deliver healthcare to the unhealthy, and strongly reject the 2% death rate associated with hospitalization. Strong consideration must be given to ambulatory healthcare delivery models that can achieve the same positive outcomes as inpatient facilities, but without the added risks.
To that end, here are some basic recommendations that will undoubtedly help lower the numbers.
1. HAND WASHING
Hand washing is the single most important measure healthcare providers can do to reduce the risks of transmitting skin microorganisms from one person to another, or from one site to another on the same patient.
That means washing hands as promptly as possible between patient contacts and after contact with blood, body fluids, secretions, excretions, and equipment or articles contaminated by them. It’s also important to use the proper time and technique when hand washing. Below are two instructional posters courtesy of the World Health Organization.
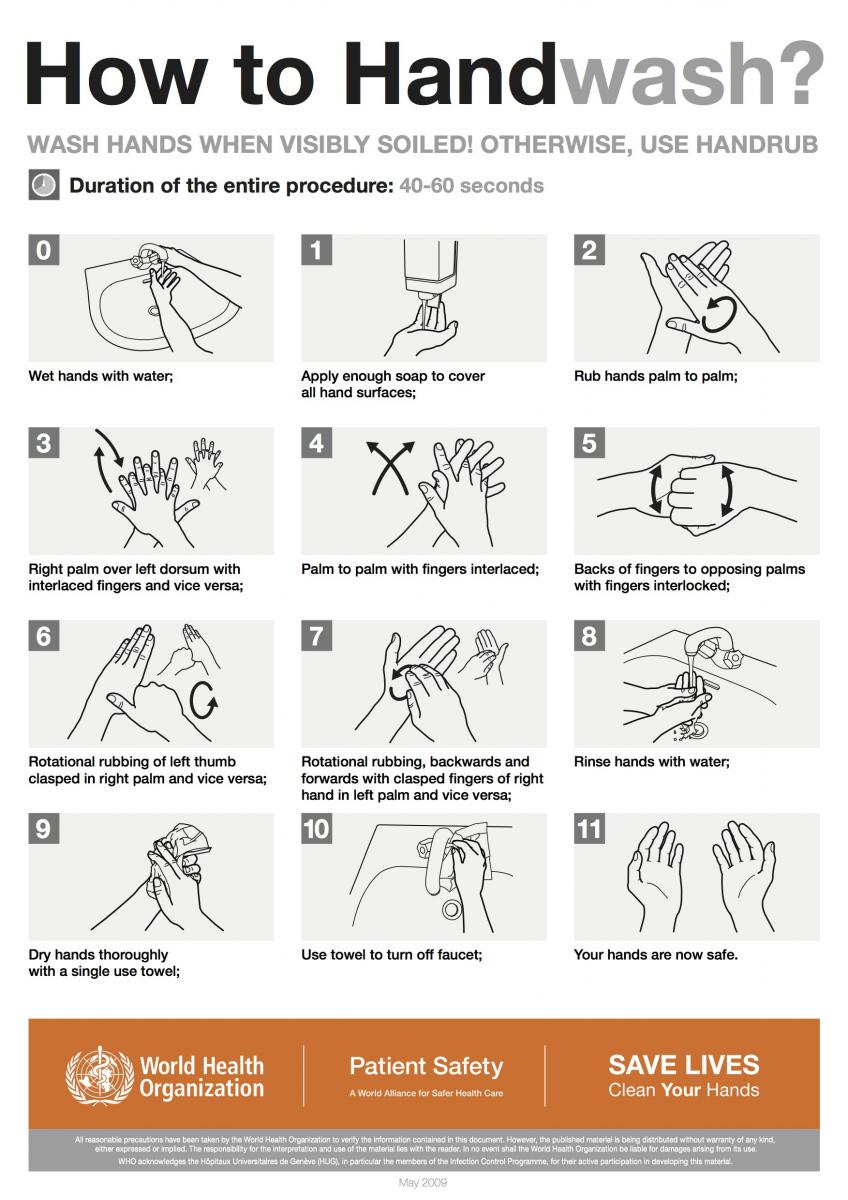
Note that the guidelines suggest washing hands when they’re visibly soiled and then to use an alcohol-based hand rub to supplement (see below). According to the CDC, many studies have found that sanitizers with an alcohol concentration between 60-95% are more effective at killing germs than those with a lower alcohol concentration or non-alcohol-based sanitizers. Non-alcohol-based hand sanitizers may not work well for all germs, they can cause germs to develop resistance to the sanitizing agent and may only reduce the growth of germs rather than kill them outright. Also, they may be more likely to irritate the skin than alcohol-based hand sanitizers.
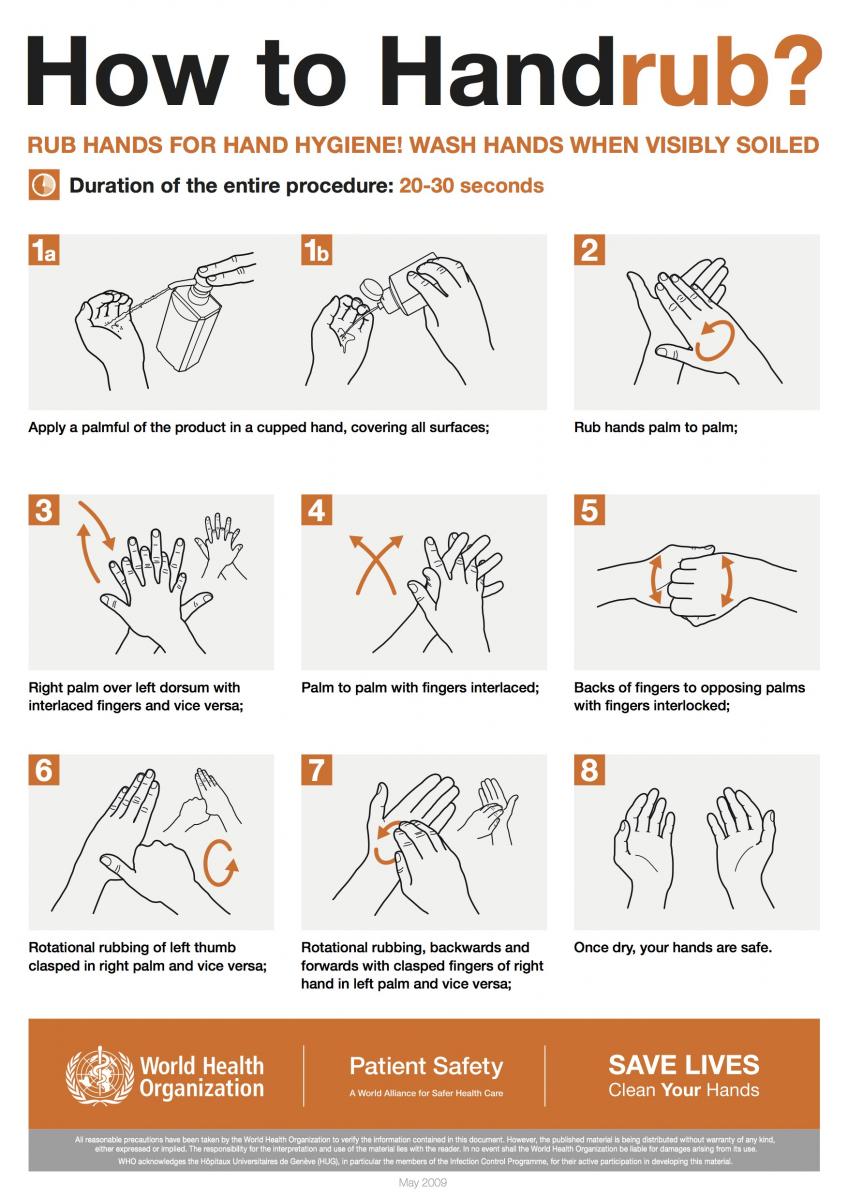
Here, it’s important to note that alcohol-based sanitizers can quickly reduce the number of microbes on hands in some situations, but sanitizers do not eliminate all types of germs. That’s because although alcohol-based hand sanitizers can inactivate many types of microbes when used correctly, people may not use a large enough volume of the sanitizers or may wipe it off before it has dried, rendering them less effective.
Additionally, soap and water are more effective than hand sanitizers at removing or inactivating certain kinds of germs including Cryptosporidium, norovirus and Clostridium difficile.
Essentially, what works best to reduce the spread of germs in healthcare settings in terms of hand hygiene is a combination of thorough, soap and water hand washing and using an alcohol-based hand rub.
This principle not only applies to healthcare workers, but to patients and visitors as well. Patients and visitors, after all, have bacteria colonizing on them just like everyone else, and they touch surfaces within healthcare settings. So it makes sense to teach and encourage them to use good hand hygiene—to be active participants in the reduction and elimination of healthcare-acquired infections.
2. GLOVES
Gloves are important in reducing the risks of transmission of microorganisms. They’re worn for three critical reasons in healthcare settings. First, they provide a protective barrier when touching blood, other body fluids, mucus membranes and non-intact skin.
Second, gloves also reduce the possibility that microorganisms from one patient or healthcare-related items (such as catheters, IV drip tubes and stethoscopes) could be transmitted to other patients during patient-care procedures.
Lastly, gloves reduce the likelihood that the hands of personnel contaminated with microorganisms from a patient can be transmitted to another patient. Here, it’s important to reiterate that gloves must be changed between patient contacts, and hands should be washed after gloves are removed.
It’s also important to note that wearing gloves does not replace the need for hand washing because gloves may have small defects or they may be torn during use. Plus, hands can become contaminated during glove removal. Obviously, failing to change gloves between patient contacts is an infection control hazard.
 Proper glove removal so germs are not transmitted to the hands.
Proper glove removal so germs are not transmitted to the hands.
3. SANITIZING TOUCH SURFACES
Some germs can live for long periods of time on surfaces within healthcare settings, particularly those surfaces that are frequently touched by healthcare personnel. Sanitizing these surfaces on a regular basis is critical to reducing the number of hospital-acquired infections.
Touch surfaces commonly found in hospital rooms, such as bed rails, call buttons, touch plates, chairs, door handles, light switches, grab rails, intravenous poles, dispensers (alcohol gel, paper towel, soap), dressing trolleys, and counter and table tops are known to be contaminated with staphylococcus, MRSA and vancomycin-resistant enterococcus (VRE).
Objects in closest proximity to patients have the highest levels of MRSA and VRE. This is why touch surfaces in hospital rooms can serve as sources, or reservoirs, for the spread of bacteria from the hands of healthcare workers and visitors to patients.
 Common sites in a hospital setting where germs can be acquired through touch.
Common sites in a hospital setting where germs can be acquired through touch.
4. SPEAK UP!
It’s up to healthcare workers to do all they can to stem the onslaught of healthcare-acquired infections including hand washing, gloving up and making sure surfaces are disinfected. Conversely, it’s up to patients and their advocates to speak up when they see these guidelines not being followed.
Patients have to speak up.
If a healthcare worker is about to touch you and you haven’t seen him/her either wash their hands or rub them properly with an antibacterial hand sanitizer, you must speak up. It may sound dramatic, but considering the facts and figures stated above, this could be a matter of life and death. Patients simply cannot accept the risk of being silent in these situations.
Patients have to ask questions even though it’s often the most difficult thing for a patient to do. How long will this catheter stay in? How often will the catheter be changed? What can I do to make sure I don’t get a surgical site infection?
The Importance of Reporting Adverse Healthcare Incidents
Reducing the number of healthcare-acquired infections is a primary concern for hospitals, outpatient centers and long-term care facilities alike. And while some recent reports suggest the numbers may have declined slightly, there is also a big problem with getting hospital workers to recognize adverse healthcare incidents, including infections, when they happen, and then to follow through with reporting those incidents to management.
In fact, according to the January, 2012 report by the Department of Health and Human Services Office of Inspector General, hospital staff did not report up to 86% of adverse events (including infections) to incident reporting systems, partly because of staff misperceptions about what constitutes an adverse event.
Clearly, much work needs to be done in order to improve patient safety and reduce the number of healthcare-acquired infections. And it all begins with the most basic action any healthcare worker can do: wash their hands.
Image Credits
Centers for Disease Control and Prevention (www.cdc.gov)
World Health Organization (WHO) (www.who.org)
About the Author
Dr. Bruce Ruben is the Founder and Medical Director of Encompass HealthCare, located in West Bloomfield, Michigan. Encompass Healthcare is an outpatient facility featuring advanced wound care, IV antibiotic therapies, hyperbaric oxygen treatment, nutritional assessment, and other treatment modalities. Dr. Ruben is board certified in Internal Medicine, Infectious Disease, and in Undersea and Hyperbaric Medicine. He is a member of the Medical and Scientific Advisory Committee and National Spinal Cord Injury Association (NSCIA) board.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, Kestrel Health Information, Inc., its affiliates, or subsidiary companies.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.








Follow WoundSource
Tweets by WoundSource