What Is a Venous Leg Ulcer?
January 31, 2019
A venous leg ulcer (VLU) is caused by vein disease that primarily affects older adults. As a prevalent problem among older patients, providing care for individuals with VLUs is time-consuming and costly. The direct costs vary from country to country, with reporting numbers of €800 monthly in Germany.1 Statistics report $2,500 monthly in the United States per patient,2 and given the chronic nature of VLUs, the cumulative costs per patient increase rapidly. A VLU is an open skin lesion of the leg or foot (gaiter area) that occurs in an area affected by venous hypertension. Generally speaking, the ulcer must be present for at least four weeks before it is considered chronic and a VLU.2 This article provides an overview of the etiology, risk factors, symptoms, and characteristics of VLUs.
Etiology of Venous Leg Ulcers
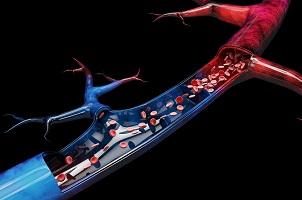
VLUs can have "pure" or "mixed" venous causes. A pure VLU occurs when there is directed axial great saphenous vein reflux or incompetent perforator reflux directly into the ulcer bed. Mixed etiology is considered when there is a venous cause, in addition to arterial ischemia, hypersensitive skin, lymphedema, local trauma, and infection, among other conditions. This distinction is crucial because there are often differences in healing times and the efficacy of surgical interventions.3 VLUs generally occur in individuals with chronic venous insufficiency (CVI), a condition that also results in varicose veins and skin changes. Both reflux and obstruction are contributors to CVI, and although reflux has a higher prevalence in patients with CVI, obstruction from secondary venous disease and valvular reflux contribute to a more rapid and higher change of progression of ulceration.4 The condition leads to increased ambulatory pressure.
Venous Leg Ulcer Risk Factors
There are multiple identified risk factors that are associated with the development of VLUs. The genetic makeup and environmental conditions can influence both the predisposition of an individual to develop venous disease and the progression and perpetuation of the disease.5 Hemochromatosis C282Y (HFE) and some factor VIII V34L gene variations may be associated with increased risk and more severe forms of CVI, causing an increased size of venous ulcers.6 Other risk factors, including family history, age, sex, pregnancy, estrogen, patterns of sitting and standing, posture and obesity, may indicate a predisposition for CVI.5
Symptoms and Characteristics of Venous Leg Ulcers
Venous disorders manifest in multiple ways, including presentation with varicose veins and vein-related skin trophic changes, ranging from pigmented dermatitis to lipodermatosclerosis, atrophie blanche, and the presence of the ulcer itself. Patients may experience a variety of symptoms including aching, pain, feeling a burning sensation, cramping, fatigue, restless legs, skin irritation, muscle cramps, heaviness, tension, feelings of swelling, and itching.7 For a leg ulcer to be classified as a VLU, the clinical symptoms should be consistent with CVI, and a full evaluation should be able to differentiate primary, secondary, or congenital venous conditions and establish whether venous obstruction, reflux, or both are present.2
Treatment of Venous Leg Ulcers
Venous symptoms tend to get worse with prolonged sitting or standing and can be relieved by resting or elevating the leg. Treatments for VLUs include compression therapy, topical treatments, debridement, oral antibiotics, sclerotherapy, and surgery, depending on the severity and chronicity of the ulcer.8 Combining appropriate compression therapy with an ideal wound healing environment is requisite for successful treatment of VLUs. Compression therapy is the first line of treatment to combat the pathology of CVI and its sequelae. Compression works by assisting blood to return to the venous system through application of external forces via dressings which form a cylindrical compression gradient over the lower extremity.
Therapeutic compression acts as a barrier to increased edema fluid in addition to decreasing existing tissue edema. Another function of compression works through providing resistance to the calf muscle pump; an ineffective calf muscle pump is another physiologic factor in CVI, as this is a primary mechanism aiding with returning venous blood to the heart. Resolution of edema can mitigate local inflammatory effects by reducing venous pressures and concentration of pro-inflammatory cytokines.9 Chronic VLUs are the most common wounds seen in health care settings. This wound type is very time-consuming, challenging, and a burden to health care costs. Effective VLU management should include partnership with the patient when deciding on the best treatment to prevent recurrence. Essential management strategies will help aid in edema management and healing outcomes.
References
1. Van Gent BW, Wilschut ED, Wittens CW. Management of venous ulcer disease. BMJ. 2010;341:1092–6.
2. O’Donnell TF Jr, Passman MA, Marston WA, et al. Management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2014;60(2):3S–59S.
3. Mosti G, Iabichella ML, Partsch H. Compression therapy in mixed ulcers increases venous output and arterial perfusion. J Vasc Surg. 2012;55(1):122–8.
4. Labropoulos N, Gasparis AP, Pefanis D, Leon LR Jr, Tassiopoulos AK. Secondary chronic venous disease progresses faster than primary. J Vasc Surg. 2009;49(3):704–10.
5. Anwar MA, Georgiadis KA, Shalhoub J, Lim CS, Gohel MS, Davies AH. A review of familial, genetic and congenital aspects of primary varicose vein disease. Circ Cardiovasc Genet . 2012;5(4):460–6.
6. Zamboni P, Tognazzo S, Izzo M, et al. Hemochromatosis C282Y gene mutation increases the risk of venous leg ulceration. J Vasc Surg. 2005;42(2):309–14.
7. Carpentier PH, Maricq HR, Biro C, Ponçot-Makinen CO, Franco A. Prevalence, risk factors, and clinical patters of chronic venous disorders of lower limbs: a population-based study in France. J Vasc Surg. 2004;40(4):650–9.
8. Rai R. Standard guidelines for management of venous leg ulcer. Indian Dermatol Online J. 2014;5(3):408–11.
9. Harding, K. Simplifying venous leg ulcer management: consensus recommendations. Wounds UK. 2015. Available at https://www.wounds-uk.com/resources/details/simplifying-venous-leg-ulce… [Accessed January 9, 2019].
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











Follow WoundSource
Tweets by WoundSource