Wound Bed Preparation and Therapeutic Interventions: Optimizing Moisture Balance
July 1, 2018
Before embarking on the journey of wound bed preparation, the goals for wound care should be carefully considered. A realistic look at the goals and expectations from the perspective of the patient as well as the wound care team is the first step in developing and implementing the appropriate plan of care. Is the wound healable? This requires that the individual's body can support the phases of wound healing in an expected time frame.
Treatment should be aggressive to prevent any delay in the healing process that would stall wound healing or lead the wound to become chronic. Is maintenance the goal? If so, then efforts should focus on keeping the wound from deteriorating by providing comprehensive wound care. Is hospice or palliative care the goal? If the wound is not expected to heal and the individual’s body cannot support the phases of wound healing within an expected time frame, then comfort measures are more important than a cure.1 All parties should be on the same page with goals and objectives so they are working in tandem toward the best outcome for the individual patient.
TIME Wound Management Model
TIME is a mnemonic that embraces the wound bed preparation model. By spelling the word time, TIME, the clinician can advance through the assessment process to keep the wound progressing, take a chronic or delayed wound and get it moving forward again, or maintain a wound that will most likely not heal and prevent it from worsening.2 The TIME wound bed preparation framework is a practical approach, especially for health care practitioners, when conducting wound assessments, identifying barriers to healing, and developing a comprehensive plan of care. It is also a reminder to treat the whole patient, not just the hole in the patient.
Wound Moisture Management
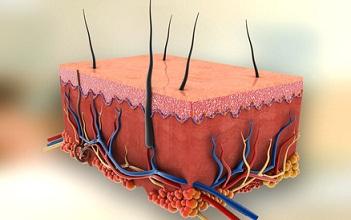
Although it can be a challenge, it is important to have and maintain moisture balance in a wound bed, to enable cells such as fibroblasts and keratinocytes, along with growth factors and cytokines, to move across the wound bed. Too much moisture can lead to periwound maceration and skin breakdown, whereas too little moisture can impair cellular activities and cause desiccation, which promotes necrotic tissue formation resulting in poor wound healing. Early studies on blisters showed that maintaining a moist wound healing environment provided continuous autolytic debridement, promotion of granulation tissue formation, faster healing, and less scarring, pain, and bioburden.3
A moist wound environment is maintained primarily by appropriate dressings, with occlusive, semiocclusive, absorptive, hydrating, and hemostatic characteristics, depending on the surface exudate and the need for moisture balance in the wound bed. Transparent films, hydrogels, hydrocolloids, foams, alginates and gelling fibers, and super absorbent polymers will aid in maintaining the delicate balance needed for a moist wound healing environment.4 Transparent films are used for dry to moist wounds. They provide a waterproof, bacterial barrier, and they are 100% adhesive.
Transparent films are not recommended for skin tears because are not occlusive, given that they have the ability to transfer moisture vapor. These dressings are indicated for prevention or as a primary or secondary dressing. They can be left in place for up to seven days. They come with and without antimicrobial features, and the moisture level is appropriate if the drainage stays within the confines of the dressing. Hydrogels are water-based products that come in amorphous or sheet versions. One of the features of hydrogel dressings is their ability to donate moisture to a relatively dry wound.
The gel sheets may have features that allow them to either donate or absorb varying degrees of moisture. These dressings can contain different ingredients, including antimicrobial silver; they are indicated for either partial- or full-thickness wounds and are excellent for use when gentle adhesion is required. Depending on the viscosity of the gel, these dressings can be worn for up to seven days. Hydrocolloid dressings are indicated for dry to moderately draining wounds and are 100% adhesive. They provide a waterproof bacterial barrier, come in occlusive or semiocclusive dressing types, and are indicated for prevention on at-risk areas or on partial-thickness or shallow full-thickness wounds. These dressings can be left in place for up to seven days; however, they should be used with caution in immunocompromised patients or on those at risk for skin tears.
Foam dressings are designed for use with minimal to heavily draining partial- or full-thickness wounds or as a preventive measure on high-risk areas for pressure or shear. These dressings are available with and without antimicrobial properties and may help to prevent hypergranulation tissue formation. Foam dressings can be left in place for up to seven days or changed sooner based on “strike through” or visible saturation. They can be used alone as a primary dressing or as a secondary dressing in combination with alginates, gelling fibers, or other primary dressing types. This may enhance wear time and decrease the necessity for more frequent dressing changes. Alginates and gelling fibers are non-woven, non-adhesive pads, ribbons, and ropes composed of natural polysaccharide fibers derived from seaweed, carboxymethylcellulose, and chitosans. They are designed to manage moderate to heavy drainage.
These dressings form a moist gel through a process of ion exchange. They also come with or without antimicrobial properties and can be left in place for up to seven days. Frequency of dressing change is determined by strike through on the secondary dressing, and if they are used in combination with foams, the wear time may be increased. Alginates and gelling fibers are indicated for all types of partial- and full-thickness wounds, including surgical wounds. However, if there is concern about retrieving the dressing from a cavity, tunnel, or dead space, do not place these dressings in the wound bed. Alginates should not be used with hydrogels. Another option for addressing moisture balance is the super absorbent polymer dressing category recommended for moderately to heavily draining wounds. They are multilayer non-adherent wound covers combined with highly absorptive polymers that act as a super absorbent core. These polymers lock away exudate by converting it into a gel. Locking excess moisture away from the wound bed helps to protect the periwound skin from maceration. Some versions of absorbent dressings vertically wick the fluid through the dressing into the outer dressing. They are indicated for all types of partial- and full-thickness wounds and may be worn for up to seven days.
TIME Helps Heal Wounds
Understanding the importance of appropriate wound bed preparation is a key component in achieving positive wound outcomes. TIME should be understood not just as a mnemonic but also as guidance to best practice in wound management. Utilizing each component, clinicians are able to choose the appropriate products and therapies to yield the best and most cost-effective outcome based on the goals and objectives agreed on by the patient and health care provider alike.
References
1. Powers JG, Higham C, Broussard K, Phillips T. Wound healing and treating wounds: Chronic wound care and management. J Am Acad Dermatol. 2016;74(4):607–25. Available at: https://www.jaad.org/article/S0190-9622(15)02183-0/pdf. Accessed June 20, 2018.
2. Ousey K, Rogers AA, Rippon MG. Hydro-responsive wound dressings simplify T.I.M.E. wound management framework. Br J Community Nurs. 2016;21(12):29–39. Available at: https://doi.org/10.12968/bjcn.2016.21.Sup12.S39. Accessed June 20, 2018.
3. Kahn S. Highlights from the advanced wound healing stream at the LINK Congress. Br J Nurs. 2017;26(20):34–5. Available at: https://www.magonlinelibrary.com/doi/abs/10.12968/bjon.2017.26.Sup20.S3…. Accessed June 20, 2018.
4. Dabiri G, Damstetter E, Phillips T. Choosing a wound dressing based on common wound characteristics. Adv Wound Care. 2016;5(1):32–41. Available at: https://doi.org/10.1089/wound.2014.0586. Accessed June 20, 2018.
Suggested Reading
McLain NEM, Moore ZEH. Wound cleansing for treating venous leg ulcers. Cochrane Database Syst Rev. 2015;(4):CD011675. doi: 10.1002/14651858.CD011675. Available at: http://cochranelibrary-wiley.com/enhanced/exportCitation/doi/10.1002/14…. Accessed June 20, 2018.
Sibbald RG, Elliott JA, Ayello EA, Somayaji R. Optimizing the moisture management tightrope with wound bed preparation 2015©. Wound Healing Southern Africa. 2016;9(1):9–15. Available at: https://journals.co.za/content/mp_whsa/9/1/EJC190662. Accessed June 20, 2018.
Spinchler A, Hurwitz BL, Armstrong DG, Lipsky BA. Microbiology of diabetic foot infections: from Louis Pasteur to ‘crime scene investigation’. BMC Med. 2015;13(2):1–13. Available at: https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-014-0232-0. Accessed June 20, 2018.
Yun X, Samad A, Milica R Biochemical and biophysical cues in matrix design for chronic and diabetic wound treatment. Tissue Eng Part B Rev. 2017;23(1):9–26. Available at: https://www.liebertpub.com/toc/teb/23/1. Accessed June 20, 2018.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











Follow WoundSource
Tweets by WoundSource