Surgical Wound Management: Preventing SSI in Colorectal Surgery
April 18, 2018
By Samantha Kuplicki MSN, APRN-CNS, AGNCS-BC, CWCN-AP, CWS, RNFA, CFCN
Surgical site infections (SSIs) are the most frequent complications in colorectal surgery procedures, with the documented incidence in literature ranging from 3% to 30%. (And, as we discussed in a previous installment, patient-specific risk factors can be the most challenging to control.) In response to these data, the American College of Surgeons and The Joint Commission’s Center for Transforming Healthcare launched a collaborative effort in 2012 to reduce colorectal SSIs.
After an observation of a two-year effort, an overall 32% reduction in all-classification colorectal SSIs was observed, totaling over $3 million in cost savings. This could translate to the prevention of over 30,000 SSIs and $800 million in cost savings when these results are applied nationally. This reduction in SSI incidence was achieved by addressing the observed SSI rate as a function of eight specific “risk points” to address in the operative process (preoperative, intraoperative, postoperative, discharge).
Addressing the Risk Points
1. Modifiable / Nonmodifiable Risk Factors
- Non-modifiable risk factors: advanced age, pre-existing conditions such as cancer, past medical interventions (e.g., radiation), and personal history/propensity for actual infection.
- Modifiable risk factors: diabetes mellitus (short-term normalization of blood glucose values is more important than control of HgB A1c), obesity, alcohol abuse, tobacco abuse (current or history of), serum albumin (below 3.5 mg/dL: normal 3.5–5.0 mg/dL), serum bilirubin (total: below 1.0 mg/dL), immunosuppression.
2. Surgical Consult and Preadmission Testing
- During surgical planning, the patient can be preoperatively optimized, including patient education about SSIs and measures for prevention. It is crucial to individualize patient and caregiver education utilizing validated techniques that match their learning style, including techniques such as teachback, and written instruction. Topics should include, at a minimum, hand hygiene and skin care in the surgical area preoperatively (no shaving or scrubbing/abrading of the skin, etc).
3. Admission and Transfer Procedures
- Is the surgical procedure elective or urgent/emergent? Assessment and case preparation will vary based on this status. For elective cases, many of the preoperative modifiable risk factors can be optimized, and the patient has the opportunity to receive adequate education regarding SSI prevention and any preoperative instructions specific to the condition. In cases of urgent or emergent procedures, especially those involving gross contamination, the range of interventions for prevention of SSIs becomes more limited.
4. Preoperative Holding Areas
- Preoperative skin preparation should be standardized, including orders for patient skin cleansing and hair removal (it is recommended that clipping of the operative site occur in the preoperative area versus the OR).
- EHR should automatically prompt an order for skin cleansing in preoperative/holding for patients who are at high risk for SSIs or those with a BMI higher than 30.
- Maintenance of normothermia should begin preoperatively.
5. Preoperative/Operating Room
- Surgical prep should be standardized regarding the type of preparatory agent and who is allowed to perform the preparation.
- Use a weight-based antibiotic dosing protocol within one hour of the first incision, and have the EHR prompt for redosing in the three- to four-hour range, as determined by the individual facility.
- Surgical technique, instrument handling, and teamwork: double glove, use a wound protector, standardize the setup and the instrumentation set used for clean versus “dirty” parts of the surgical procedure, establish standardized closing process including pre-closure subcutaneous tissue irrigation with at least 2L of NS.
- Continue aggressive monitoring and care of blood glucose and maintenance of normothermia.
- Administer a high fraction of inspired oxygen (>80%) during surgery (15L nonrebreather mask for 4 hours)
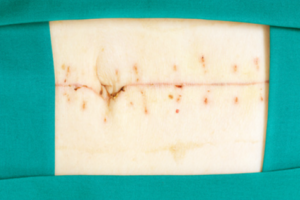
- Apply a standardized antimicrobial dressing (supported by ACS, although the National Guideline Clearinghouse specifically recommends against standard application of antimicrobial dressing for incisions left to close by primary intention for reasons of microbial resistance and cost).
6. Postoperative Recovery, PACU-Floor/ICU
- Postoperative care management should include reinforcement of hygiene practices, postoperative teaching, and incision care instructions.
- Administer a high fraction of inspired oxygen (>80%) after surgery (15L nonrebreather mask for 4 hours).
- Also standardize who will remove the operative dressing because the initial incision assessment is crucial to identification of complications. The first dressing is ideally removed by the primary service providers for this reason.
- Establish protocol for contaminated colorectal surgical wounds (National Guideline Clearinghouse states no supporting evidence for engaging wound specialist in care of patient with non-healing surgical wound, but does recommend wound specialist involvement for complex wound therapies such as negative pressure wound therapy [NPWT] and presence of ostomies or fistulas).
7. Postoperative Care, Patient Care Unit, and Discharge
- This involves incision or wound management and ongoing patient education as listed in the earlier phases, with increased emphasis on sequential discharge day events (e.g., day one out of the hospital, expect certain events, observe for specific changes that could potentially indicate infection, and when to notify provider).
- Have nurses make a follow-up phone call to patients within one week after discharge from the hospital.
8. Post-Discharge and 30-Day Follow-Up
- Evaluate length of stay for any patient with postoperative complications, including need for reoperation and any incisional complications or wound occurrence.
Want to read more about the current recommendations and guidelines for reducing SSIs? Click Here.
Utilizing SSI "Bundles"
Failures at each specific “risk point” that increase SSI risk propagate the targeted solutions listed earlier. As many studies have identified, there are numerous patient-, disease-, and procedure-specific variables in the development of SSIs in colorectal procedures; therefore, a multifaceted approach is required for prevention. Surgeon, anesthesia provider, advanced practice providers, OR staff, pharmacy staff, infection control specialists, unit or house nursing, and other patient care staff must collaborate to achieve best outcomes.
New evidence will beget new recommendations, and it is coming down the pike at increasing speed. A recent article in Ostomy Wound Management suggests that male sex, non-utilization of SSI bundle, and hypoalbuminemia (<3.5 g/dL) were independent predictors of wound complications after colorectal surgical procedures. In this specific study, implementation of an SSI bundle decreased wound complication rates. The use of bundles inclusive of protocols and standardization of clinical practices has been a ubiquitous, permeating theme in almost every source of literature related to SSI prevention. No specific bundle is identified as superior, but rather the presence and application of a standardized set of literature-validated practices decrease observed SSI rates.
The use of bundles can be a dynamic process because the patient population varies by geographical area, and certain aspects of a bundle can require more emphasis than others. In light of this evidence, I urge all clinicians, wound specialists, and general practice alike to become empowered with the knowledge you have garnered by reading this today and speak with key individuals at your organization about developing an SSI bundle tailored to your facility, by addressing each of the risk points discussed earlier. Knowledge is power, and a most egregious error is not learning and making changes based on what you know. And of course, I’ll leave you with a bit of wisdom from one of my favorite fictitious characters:
“Evolution forged the entirety of sentient life on this planet using only one tool: the mistake.”
-Dr. Robert Ford, HBO’s Westworld
References
1. Reducing Colorectal Surgical Site Infections. Joint Commission Center for Transforming Health Care. 2014. Retrieved April 17, 2018. https://www.centerfortransforminghealthcare.org/assets/4/6/SSI_storyboa… .
2. Surgical site infection: prevention and treatment of surgical site infection. (n.d.). Retrieved April 17, 2018, from https://www.guideline.gov/summaries/summary/13416/surgical-site-infecti…
3. Lutfiyya W, Parsons D, Breen J. A colorectal “care bundle” to reduce surgical site infections in colorectal surgeries: a single-center experience. Perm J. 2012;16(3):10–16. Retrieved on April 17, 2018. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3442755/.
4. Keenan JE, Speicher PJ, Thacker JKM, Walter M, Kuchibhatla M, Mantyh CR. The preventive surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg. 2014;149(10):1045–1052. doi:10.1001/jamasurg.2014.346. Retrieved on April 17, 2018. https://www.ncbi.nlm.nih.gov/m/pubmed/25163027/.
5. Gachabayov M, You K, Sullivan R, Bergamaschi R. Surgical site infection: prevention and treatment of surgical site infection. Ostomy Wound Manage. 2018;64(4). Retrieved April 17, 2018, from https://www.guideline.gov/summaries/summary/13416/surgical-site-infecti…
About the Author
Samantha Kuplicki is an Advanced Practice Registered Nurse and a Board Certified Clinical Nurse Specialist in Adult Gerontology. Additionally, she is dual board certified in Wound Care by both the American Board of Wound Management as a Certified Wound Specialist (CWS) and by the Wound, Ostomy and Continence Nursing Certification Board as an Advanced Practice Certified Wound Care Nurse (CWCN-AP) and Certified Foot Care Nurse (CFCN). She serves on the American Board of Wound Management (ABWM) Examination Committee, and also volunteers for the Association for the Advancement of Wound Care. Samantha’s clinical experience involves a wide variety of settings including long term care, acute care, outpatient clinics, and travel nursing. She is experienced in wound care consulting, facility and provider billing and coding, policy/procedure drafting, and has expanded her role in patient care as an RNFA (Registered Nurse First Assistant in surgery). Samantha has an intense passion for caring for patients with wound and general surgical needs. She enjoys participating in causes that further the practice of skin and wound care, including educating medical professionals, patients, and caregivers alike.
The views and opinions expressed in this content are solely those of the contributor, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.