Understanding the Role of the Continence Nurse, Reasons to Certify, and Practice Questions
June 13, 2019
Part 2 in a multi-part series reviewing different types of certification and providing tips and practice questions. Read Part 1 Here.
Not many people wake up one day and say, "Wow, I really want to be a continence nurse!" In fact, sometimes people don't even really understand what a continence nurse is, their role, or the specialty in general. I often tell nurses that although we may not all hold certification, every nurse should be a continence nurse, especially in the long-term care setting.
Think about it. As patients age, things change... some processes slow down, medications may be absorbed differently or prescribed at a "geriatric dose," and lab values may reflect chronic changes of aging. Additionally, bones and muscles change as a result of aging, and the impact of any past surgeries or procedures may start to take a toll on the body. However, just because we get older doesn't mean that we should expect to become incontinent. With that being said, it is important that every nurse empowers their patient to be as independent as able, assists with toileting, implements a toileting schedule, checks for incontinence during rounding, and puts interventions into place to help manage skin breakdown from moisture. It is also very important to understand the cause of incontinence - that way, we are able to manage the patient and treat the underlying issue most effectively.
Roles of the Continence Nurse
Becoming certified in continence... hmm. If you think about it, there are so many ways in which a continence nurse does and can directly impact quality of life for their patients each and every day. Suffering from incontinence isn't easy. It dramatically impacts quality of life, activities of daily living, ability to travel, clothing choices, determining whether or when to go out for social activities, and more. There are also many myths (and facts) about continence; as continence nurses, we are educating and empowering patients, staff, and even our family members on a regular basis.
Additionally, it's a great time to bring awareness to World Continence Week, which takes place every June. World Continence Week is a health promotion campaign, with hopes to raise awareness of incontinence and incontinence-related issues. Those patients with incontinence have support available, and it is important to bring this issue to light. Continence nursing is an important specialty and one that many of our patients often seek out throughout their life span. Therefore, it is definitely a specialty worth certifying in, and I hope to educate you briefly on the role and purpose of a continence nurse with this information, as well as provide some questions related to scope of practice and certification.
Sample Continence Nursing Questions
Question 1: Indwelling Foley catheters should be changed:
A. Weekly
B. Every six months
C. Every 28 days
D. When necessary, and not at fixed intervals
Answer: D. When necessary, and not at fixed intervals. For convenience, changing indwelling catheters seems to be ordered at Q30 day intervals; however, there is no evidence that this improves patient outcomes. Some individuals manage for months, whereas others need more frequent catheter changes. This may be related to overall health status of the patient, level of physical activity, and amount of fluid intake. Although there are different reasons and protocols in place at each institution, there is again no evidence that changing a Foley catheter Q28 or Q30 days improves patient outcomes.
Reference
Moore KN, Franklin L. Indwelling and Intermittent catheterization. In: Doughty DB, Moore KN, eds. WOCN Society core curriculum: continence management. Philadelphia, PA: Wolters Kluwer; 2016:242-243.
Question 2: A patient presents to the continence clinic for an initial evaluation of etiology and treatment options for incontinence. As she is learning about her options for management, she asks for some initial tips to better manage urinary incontinence. The continence nurse shares some tips with her, including:
A. Reduce alcohol and caffeine intake.
B. Attempt weight loss if overweight because this puts pressure on the pelvic floor.
C. Keep a bladder diary to understand urinary patterns.
D. All of the above
Answer: D. All of the above. Reducing alcohol and caffeine intake, attempting weight loss, and keeping a bladder diary are all appropriate interventions to better manage life with urinary incontinence. Some additional tips include avoiding clothing that is tight around the abdomen, keeping a change of clothes or extra supplies for containment in the car, and reaching out to your health care team for additional support groups. It is important to take an interprofessional approach to incontinence management and determine the etiology or cause of the incontinence. Once the cause of incontinence is determined, it will be more effectively managed.
Reference
The Urology Foundation. World continence week 2019. https://www.theurologyfoundation.org/get-involved/tuf-campaign-focus. Accessed May 29, 2019.
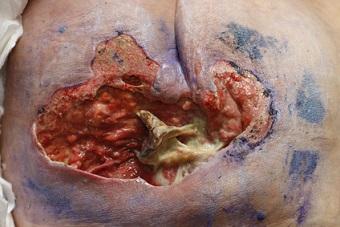
Question 3: This type of incontinence is usually caused by an acute illness or change in mental status. Management is focused on correcting the underlying disease process, containment of stool, and skin protection or prevention of skin breakdown.
A. Chronic fecal incontinence
B. Transient fecal incontinence
C. Urge incontinence
D. Passive incontinence
Answer: B. Transient fecal incontinence (FI). Transient FI is usually caused by a disease or intestinal illness, resulting in incontinence of loose stools. Although transient incontinence may have an urge FI component, urge FI is typically caused by external sphincter dysfunction, a colorectal motility disorder, or reduced capacity of the rectal cavity. Passive FI involves the leakage of stool, unrecognized by the patient. This typically happens in patients with dementia or with sensorimotor dysfunction. Chronic FI does not typically have a reversible cause, like transient FI (e.g., gastrointestinal illness, acute disease process).
Reference
Callan LL, Willson M. Fecal incontinence: pathology, assessment, and management. In: Doughty DB, Moore KN, eds. WOCN Society core curriculum: continence management. Philadelphia, PA: Wolters Kluwer; 2016:299-302.
Conclusion
As with any certification exam, be sure to explore the certifying body's website and identify the exam outline, the recommended study materials, and the availability of practice questions. Also, identify your own learning style and the types of practice exams available to meet your learning needs (e.g., hard copy, online testing, mobile apps, etc.).
Next, we will explore preparing for and understanding ostomy certification and the significance of the ostomy specialist in managing a sometimes vulnerable population.
Suggested Reading
Callan LL, Willson M. Fecal incontinence: pathology, assessment, and management. In: Doughty DB, Moore KN, eds. WOCN Society core curriculum: continence management. Philadelphia, PA: Wolters Kluwer; 2016:299-302.
Moore KN, Franklin L. Indwelling and intermittent catheterization. In: Doughty DB, Moore KN, eds. WOCN Society core curriculum: continence management. Philadelphia, PA: Wolters Kluwer; 2016:242-243.
The Urology Foundation. World continence week 2019. https://www.theurologyfoundation.org/get-involved/tuf-campaign-focus. Accessed May 29, 2019.
About the Author
Holly is a board certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this content are solely those of the contributor, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.