Accurately Identifying Wound Etiology by Tissue Type and Appearance
October 22, 2020
Identifying wound etiology before initiating topical treatment is important. Additionally, correctly documenting wound etiology is significant in health care settings for many reasons. Accurate documentation and appropriate topical treatment are two critical components of a strong wound treatment plan and program. Bedside staff members should be comfortable with describing wounds, tissue types, and differentiating wound etiologies.
Training should be provided by the certified wound care clinician, along with follow-up (chart reviews and documentation checks, one-on-one education as needed, and routine competency or education days). Additionally, the wound care clinician should be able to develop an appropriate treatment plan based on wound etiology, by involving additional disciplines as needed to best treat the whole patient. Some common types of wounds and their distinguishing features are discussed here.
Vascular Wounds
Vascular wounds are classified into two types: venous and arterial.
Venous wounds
Venous wounds are typically seen on the lower extremities, from the knees down. These wounds are usually moist in appearance and irregularly shaped, and they are often brought on by a trigger (event)—for example, bumping the leg, an increase in edema, scratching, an insect bite, or other trauma. It is important to identify the trigger (if there is one) and accurately identify and describe the wound. These wounds typically have a moderate amount of drainage and can be painful (usually described as achy pain). Venous leg ulcers (VLUs) are often superficial wounds, but they can be full-thickness wounds that heal slowly. VLUs relate to the veins, as the name suggests, and are often exacerbated by insufficient return of blood to the heart.
Arterial wounds
Arterial wounds are ischemic ulcers, caused by a lack of blood flow to the extremity (poor tissue perfusion). Arterial ulcers are typically dry ulcers, small, usually round with regular borders. These wounds can be full-thickness and often contain necrotic tissue. Pulses may be difficult to palpate in the affected extremity, and hair loss on the legs is common. Arterial ulcers are caused by damage to or blockages in the arteries, as the name suggests, and may require surgical intervention for healing to occur.
Diagnosis and treatment
Hemosiderin staining is often seen in the lower extremities of patients with vascular wounds (venous or arterial). Venous and arterial wounds are treated very differently, so it is important to identify the type of wound correctly before initiating a treatment plan.
Diabetic Ulcers
Diabetic ulcers, as the name suggests, are seen in patients with diabetes. Diabetic foot ulcers (DFUs) are most commonly located on the plantar aspect (bottom or sole) of the foot. Diabetic patients often have neuropathy or can even be insensate in the feet or lower legs, thus causing these wounds to develop and sometimes progress to infection quickly. DFUs are partial- or full-thickness wounds, often surrounded by a "hyperkeratotic rim" or a thickened or calloused border of tissue surrounding the wound itself.
Surgical Wounds
Surgical wounds are caused during surgery. Surgical wounds are often closed with sutures, staples, or skin glue. Surgical wounds can sometimes be left open to heal by secondary intention, if they are not closed during surgery. Surgical wounds vary in shape and size depending on the location and type of operation performed. Preventing infection after surgery is important, along with routine site care. Each wound is different, and instructions are typically provided by the surgical team post-operatively.
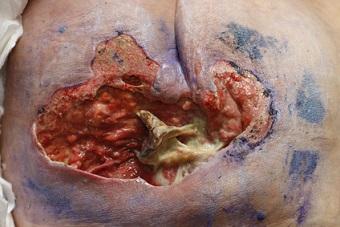
Wounds Resulting From Autoimmune Disease
Wounds caused by autoimmune diseases are sometimes initially difficult to identify. These wounds require a multidisciplinary approach to treatment and often a systemic approach to wound management. Scleroderma, pemphigoid, psoriasis or psoriatic arthritis, lupus, arthritis, and pyoderma gangrenosum are several autoimmune diseases that are often linked to chronic wounds. Wounds that are slow to heal or non-healing, difficult to treat, or not improving with standard therapy may need further investigation. Involving dermatology is often beneficial here because all of these wounds manifest differently, although they are similar to wounds in other conditions, and a tissue biopsy may be needed.
Malignant Wounds
Malignant wounds are chronic in appearance and non-healing, and they often contain friable or necrotic tissue. Malignant wounds can have an odor and moderate to heavy exudate as well. These wounds may bleed easily during cleansing or dressing changes and can be very painful. There may be induration and erythema, along with the "orange peel" appearance of skin secondary to tumor invasion and edema. Malignant wounds require a multidisciplinary approach and may be difficult to heal without systemic treatment or treatment of the cause.
Traumatic Wounds
Traumatic wounds are most commonly caused by an injury. Most frequently seen are skin tears and abrasions, especially in older adults. Traumatic wounds can also be caused by injury from a foreign body (e.g., stepping on a nail or cutting your finger with a knife). The appearance of traumatic wounds varies greatly by the cause. The etiology of these wounds is often discovered by patient interview.
Pressure Injuries
Pressure injuries are caused by unrelieved pressure, often over a bony prominence. Moisture, friction, shear, and use of medical devices can also contribute to development or delayed healing of a pressure injury. It is important to look at what is causing the pressure injury and to remove the causative or aggravating agent, to develop an effective treatment plan. Pressure injuries can be partial- or full-thickness wounds, and treatment depends on the overall patient situation and goals of care. Differentiating pressure injuries from moisture-associated skin damage and vascular wounds is important—if you're not sure, call your wound care specialist!
Wounds of Uncertain Etiology
If you're unsure of a wound's etiology, consult with your wound care specialist. Often, wounds with very different etiologies can have a similar outward appearance. It is important to identify the wound accurately and to document the correct wound etiology consistently. Wound etiology is a leading factor in developing and carrying out a holistic, effective, and evidence-based treatment plan. Involvement of the interprofessional team and close follow-up are also important. Stay tuned for Part II: Treatment Recommendations Based on Wound Etiology and Appearance.
About the Author
Holly is a board-certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











Follow WoundSource
Tweets by WoundSource