Understanding the Braden Scale: Focus on Shear and Friction (Part 5)
January 11, 2018
Part 5 in a series analyzing the use of the Braden Scale for Predicting Pressure Sore Risk® in the long-term care setting. For Part 1, click here. For Part 2, click here. For Part 3, click here. For Part 4, click here.
Friction and shear… what’s the difference and how do they cause pressure injuries? Are wounds caused by friction and shear classified as pressure injuries? What’s the easiest way to explain the differences between these critical components of the Braden Scale for Predicting Pressure Sore Risk® that are not always understood? How do I know if my patient is at risk?
When nurses hear the terms friction and shear, there’s always a component of confusion, along with grouping them as one and the same. It is confusing, documentation is usually always done at the end of the shift because patient care is a priority, and no one really has time to look up the definitions of categories of the Braden Scale… trust me, I get it.
Friction and Shear: Definitions, Comparisons, and Risk Factors in Pressure and Other Injuries
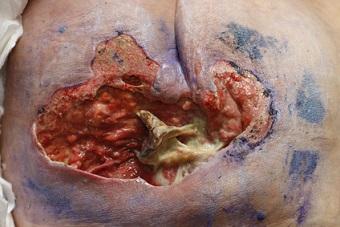
Simply put, friction and shear are similar but different—see my brief descriptions below. Friction and shear can both cause a pressure injury, but friction and shear injuries are not always and should not always be classified as pressure injuries. Picture this scenario… your patient is agitated and in restraints, his wrists are rubbing because of constant movement, and superficial abrasions are noted under the restraints… the areas are not round or punched out, and they lack characteristics of a pressure injury… they’re not over a bony prominence… and in some spots, you can actually see the skin flap that is intact or damaged—these are friction injuries. Now, with that same patient, let’s say he or she had intravenous (IV) access in place under the restraint, with an IV stabilization device and clear film dressing… the restraint was tight and caused pressure on the area… once the restraint was removed, a superficially open area shaped exactly like the IV and stabilization device was noted – this is a medical device-related pressure injury—see the difference?
Shear: Shear is a little more complicated, but still the same principles apply. Shear injuries are more often full-thickness when compared with friction injuries, but they can also be superficial. Shear injuries, in my experience, more often than not develop into pressure injuries, or in some cases are noted initially as a pressure injury related to shearing forces. It is important to look at the entire picture when determining whether or not a wound is a true pressure injury, especially when dealing with the forces of friction and shear. Shear involves gravity—think of when we hoist a patient up in the bed using a sheet instead of a repositioning sling attached to an overhead lift, and when the patient slides back down. More times than not, the patient’s skin isn’t fully lifted from the bed and linens, and this creates a force of shear from the linens and the patient’s skin moving in an opposite direction – this is shear.
Friction: Gravity is not usually involved. With shear injuries, gravity usually plays a large role in the injury. Friction and shear can both be present depending on the situation but don’t always have to be. Shear injuries more often lead to pressure injuries, but friction and shear both can cause pressure injuries. Always look at the big picture and what actually caused the wound… the root of the problem. Don’t ever hesitate to call your certified wound ostomy continence nurse specialist if you have a question, need clarification, or just aren’t quite sure… that’s what we are here for!
Braden Scale Scoring for Risk Assessment
Now, scoring the Braden Scale, what would place someone at risk in this category? First, let’s clarify: the friction and shear category of the Braden Scale has three subcategories, and the other categories have four subcategories. With friction and shear we have 1 to 3 – 1: Problem; 2: Potential Problem; 3: No apparent problem. The definitions of these categories can be explored more in depth on the scale itself, but an important principle to remember is that if your patient is not completely independent with activities of daily living and care, the patient is going to be at least a “potential problem” or potential risk for friction and shear injuries, which in turn can lead to pressure injuries.
If someone is bedbound (total care, patients with spinal cord injury, hip fractures, immobilizers, etc.), the patient is definitely going to be classified as a “problem,” placing this person at high risk for friction and shear injuries from repositioning, movement, etc. Those patients in the units in restraints or who are sedated or intubated also would meet the “problem” criteria. I always try to explain to my nurses that when people are in the hospital, they’re sick, and they’re not doing all that they used to… they’re weak and spending more time in bed. Almost every patient I have seen as an inpatient has used the elbows or heels to reposition in bed – definitely a “potential problem.”
Interventions to Prevent Friction and Shear Injuries
Taking the Braden Scale one step further, if you’ve identified that your patient is even a potential risk in this category, you need to put interventions into place. What are some interventions that could help with preventing friction and shear injuries, thereby preventing pressure injuries?
- Keep the head of the bed less than 30 degrees if and when appropriate (taking into consideration mealtimes, tube feedings, etc. – not always possible).
- If your patient requires assistance with repositioning, use a repositioning sling with an overhead lift when available. Whenever possible, be sure that your patient’s skin isn’t sliding against the linen when repositioning – shear injuries will certainly happen!
- Use the knee-gatch position on the bed as appropriate – this can prevent the patient from sliding down in the bed. Work with or consult occupational therapy or physical therapy as appropriate to determine whether this is appropriate for your patient.
- Checking placement of medical devices and turning or repositioning the patient as needed during hourly rounds. If your patient is uncomfortable, friction and shear injuries are more likely to happen.
- Always take an interprofessional approach… involve physical therapy and occupational therapy – they almost always have great suggestions to help with prevention, are the experts with seating surfaces, and are key parts of our team. Don’t forget to involve the direct caregivers in this discussion as well. Taking an interprofessional approach will help to promote more positive outcomes.
I want to thank you for joining me weekly in this five-part blog on the Braden Scale, discussing interventions along with key points for nursing staff education. Remember: prevention is key, along with working together (teamwork) to meet the needs of our patients and staff!
Note: For anyone who wishes to utilize the Braden Scale in their health care facility, you must request permission to do so. Please visit www.bradenscale.com and complete the Permission Request form.
About the Author
Holly is a board certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.











Follow WoundSource
Tweets by WoundSource