Wound Assessment, Treatment and Follow-Up
April 25, 2018
After determining our goals of wound treatment (healing, maintaining, or comfort/palliative), we need to choose a treatment that meets the needs of the wound and the patient.
Wound Assessment: Using Your Senses
When assessing a wound, we typically use three of the five senses:
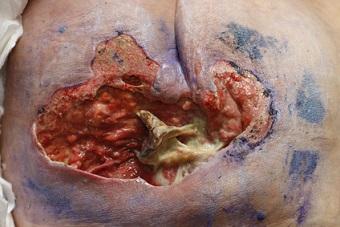
See: What does it look like? What color is the wound bed? Is there necrotic tissue? Are underlying structures exposed (bone, muscle, tendon)? Is there tunneling or undermining? What are the wound measurements (length x width x depth)? What color is the drainage? How much drainage? Is there periwound maceration (from moisture)? Epibole? Do you have photos or a prior assessment for comparison with the current assessment?
Smell: Is there an odor? Is the odor related to chronic wound drainage, autolytic debridement, infection, contamination (stool or urine), the treatment being used? Is the odor present after cleansing the wound?
Touch: Is there crepitus, induration, firmness, erythema? Can you palpate bone? Is purulent drainage expressed? Is the periwound warm? In this hypothetical case, our wound is ~5cm x 5cm x 1cm, with no tunneling or undermining, moderate serosanguinous drainage, no signs or symptoms of active infection, present over the sacrum. No bone, tendon, and muscle are currently exposed; however, they have been exposed in the past per the report you received. This is a chronic wound, present >1 year. The wound has been treated for osteomyelitis (OM) in the past, but has nothing going on currently to make us think active infection. Our goal is healing. How would you stage this wound, and what would your treatment be? Current treatment: dry gauze TID.
Stage: chronic/healing stage IV (because of past bone exposure)—remember, you can’t back stage.. once a IV, always a IV!
Wound Treatment Planning
Drainage is moderate and serosanguinous, but the dressing is being changed TID... therefore, drainage is likely going to be a large amount. Why is the wound draining so much? Is there underlying infection? Involve your interdisciplinary team here, as needed—determine whether imaging is needed, laboratory tests, etc. Remember, the gold standard for diagnosing OM is a bone biopsy... however, would this be necessary if we know that the wound was already positive for and treated for OM? Involve infectious disease, providers, and other disciplines as needed.
Some Treatment Choices:
- Alginate
- Hydrofiber
- Foam
- Composite dressing (think dressings that contain an absorptive layer, cover layer, and adhesive border)
- NPWT (negativepressure wound therapy)
Given the amount of wound drainage described in the scenario, we wouldn’t be thinking along the lines of hydrocolloids, hydrogels, transparent films, or contact layers. Because there isn’t tunneling or undermining in our wound, we probably do not need a rope or a ribbon dressing. Because there aren’t signs or symptoms of active infection, we can start with a non-antimicrobial dressing. If the wound doesn’t improve or drainage isn’t managed or if it increases, we can change our dressing to include antimicrobial properties such as silver as needed when we reassess. This narrows our selection down to: plain alginate, plain hydrofiber, NPWT, plain foam, or possibly composite dressing.
If we can complete infrequent dressing changes we can likely use a foam-bordered dressing to cover versus gauze. If we need frequent dressing changes, we will need gauze and tape. When deciding between hydrofiber and alginate there are some important things to look at… you can also refer back to my comparison chart in earlier blogs. Gelling fiber dressings are woven dressing with absorptive properties, gelling fluid on contact with the dressing. Alginates are absorptive but typically absorb less than gelling fiber dressings; they are also not woven. Both come in plain and antimicrobial formats, usually. We need a wound filler given the depth; we can’t just cover with a foam dressing.
NPWT is a more aggressive treatment. Typically, I will start with less aggressive or invasive treatments and move to more aggressive or invasive as needed. Additionally, it is important to look at and monitor laboratory results, especially nutritional markers and weight trends. Finally, before choosing and applying our dressing, we will need to decide what we will clean the wound with… plain saline versus an antiseptic or cytotoxic solution? Given our current wound description, saline seems like an appropriate choice. Because there are no periwound issues (maceration, epibole, erythema, etc.), we likely won’t need to apply a treatment to the periwound at this time.
Monitoring and Follow-Up
So, we’ll cleanse the wound, pat dry, and apply our product of choice… what do you think is the best treatment? Do you have any other suggestions? What things should we be monitoring and how often? What do you expect to happen in a week? What other things do we need to put into place? Think bed or seating surfaces, nutrition, managing friction, shear, moisture—is the patient continent? Remember the tools available to you, especially if in an inpatient setting: physical therapy, occupational therapy, dietitians, providers, general surgery, infectious disease, plastic surgery, attending providers, etc. Think of all of the categories in the Braden Scale, and be sure that you have appropriate interventions in place to meet each of this patient’s deficiencies (look back at the previous Braden mini series for suggestions). Stay tuned for my next blog to see how this wound progresses. And remember, there’s always more than one way to treat a wound!
About the Author
Holly is a board certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this content are solely those of the contributor, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.