Understanding the Braden Scale: Focus on Mobility
May 2, 2019
Part 6 in a series analyzing the use of the Braden Scale for Predicting Pressure Sore Risk® in the long-term care setting.
Part 1: Understanding the Braden Scale: Focus on Sensory Perception
Part 2: Understanding the Braden Scale: Focus on Moisture
Part 3: Understanding the Braden Scale: Focus on Nutrition
Part 4: Understanding the Braden Scale: Focus on Activity
Part 5: Understanding the Braden Scale: Focus on Shear and Friction
What is mobility? Typically, when we hear the word mobility, we think about our ability to move, with or without assistance. In a long-term care setting, we often hear the words, "mobility aids," which are typically pieces of medical equipment that are used to enhance mobility—wheelchairs, walkers, canes, power wheelchairs, crutches, and even guide dogs for those who are sight impaired. There are many intrinsic and extrinsic factors that impact one's mobility, which will be discussed in this blog.
Braden Scale Mobility Categories
When discussing the Braden Scale for Predicting Pressure Sore Risk® and mobility, there are four categories:
- Completely immobile: Unable to make any changes in body or extremity position without aid.
- Very limited: Unable to make more that slight, occasional change in body or extremity position, but require assistance for significant or frequent changes.
- Slightly limited: Able to make frequent, slight change in position.
- No limitations: Able to make frequent and significant adjustments in position unaided.
Mobility and Skin Breakdown Risk Reduction
Mobility is an important category in the Braden Scale because, as we know, the more pressure tissue is exposed to, the higher the risk is for breakdown. If someone is immobile, they are much more at risk for pressure injuries than someone who moves freely and is able to shift weight without assistance.
Immobile patients, or those with poor mobility, may benefit from a specialized support surface along with routine repositioning. An important take-away point with support surfaces is that although they are certainly beneficial in certain situations, no surface replaces turning and repositioning routinely because turning and repositioning are evidence-based, long-standing nursing interventions, supported by research to prevent pressure injuries. Turning and positioning wedges may also be helpful in promoting mobility and assisting with turning in those who are bedbound.
Specific Risks in Long-Term Care
Furthermore, in a long-term care setting, it is important to take into account that many of the residents spend a good part of their day sitting. Appointments, activities and quality of life are some of the reasons for this. Residents who are unable to walk use a wheelchair as their primary means of mobility. With that being said, it is important to understand the importance of using a seating surface in the wheelchair and implementing weight shifts every 15 minutes and as needed. Physical and occupational therapists are great resources to help with seating assessments and determining appropriate seating surfaces for chairbound patients.
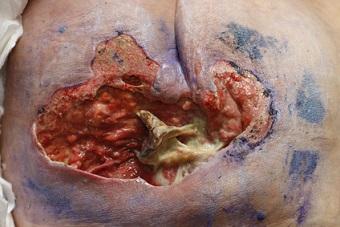
In addition to the above interventions, there are some things to keep in mind if your patient is at risk or deficient in terms of mobility on the Braden Scale. Chairbound residents are at a high risk for acquiring ischial pressure injuries because of the anatomy and pressure on the sitting bones, and bedbound patients are at higher risk for sacral, heel, occiput and vertebral pressure injuries. A routine skin assessment by nursing is an important intervention or assessment piece in order to identify at risk areas and put interventions into place. A red flag for an at-risk area is reddened skin over a bony prominence that is slow to blanch or complaint of pain verbalized by the patient. Some interventions include protective foam dressings, barrier creams and offloading. Be sure to pay close attention if the resident complains of pain over a bony prominence, and inspect the skin closely.
Again, the Braden Scale is only as accurate as the rater, and if interventions are identified but not consistently used, a pressure injury may still develop.
Conclusion
Take-away points:
- Be sure to read the definitions and identify an appropriate score for the subcategory.
- Identify and put appropriate interventions into place before pressure injuries develop and be sure that interventions are in place consistently.
- Be sure to use your evidence-based tool accurately, consistently and appropriately!
- If you're unsure of something, ask! That's what your resources are here for.
Please refer to my prior blogs in the Braden Scale series in order to put all the pieces together and promote a better understand of the Braden Scale and subcategories.
Note: For anyone who wishes to utilize the Braden Scale in their health care facility, you must request permission to do so. Please visit www.bradenscale.com and complete the Permission Request form.
About the Author
Holly is a board certified gerontological nurse and advanced practice wound, ostomy, and continence nurse coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our veterans. Holly has been practicing in WOC nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and, most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an interprofessional approach with wound care and prevention overall, and involves each member of the health care team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this content are solely those of the contributor, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.