Dressing Selection: Which Dressing to Choose?
May 31, 2018
Dressing selections can be overwhelming for clinicians and providers in health care. There are now well over 6,000 wound care products on the market. Ideally, there would be a multifunctional smart dressing that could “do it all” readily available in all settings. Unfortunately, we as health care providers know, that definitely isn’t the case. Dressing category education plays a vital role in wound management. Knowing the functionality and appropriateness of the dressing is key in enhancing the wound healing process. As wound care clinicians, we want to be in a mindset of looking at our whole patient.
However, let’s not forget the Wound Care Basics 101: wound bed preparation, monitoring, patient compliance, appropriateness of dressing, and addressing underlying factors or causes. Biofilm formation is also a culprit for impeding wound healing. Most, if not all, ulcers develop a biofilm over time. It is reported 60% to 90% of chronic wounds contain a biofilm. Therefore, selecting the appropriate dressing for effectiveness is imperative. Bioactive wound care dressings can include tissue-engineered products derived from artificial sources or natural tissues (e.g., hyaluronic acid, elastin, silicone, chitosan, alginates, collagen, antimicrobials, skin equivalents, growth factors, cell-free matrices, cell-containing matrices). The use of synthetic protein matrix and growth factors also helps drive future growth.
Dressing Selections Considerations
To select the appropriate dressing for a given wound, ask yourself the following questions:
How is the wound being cleansed with each dressing change?
Whether you are using normal saline or a non-cytotoxic wound cleanser, we must be consistent with wound cleansing for wound bed preparation.
Is the wound partial-thickness or full-thickness, with or without tunneling and undermining?
Dead space of a wound must always be loosely packed. You also want to make sure the dressing will maintain its shape to keep direct contact with the wound bed. Also, select dressings that do not fray or come apart.
How often should the dressing be changed?
If the wound is draining a scant amount, you can stretch the wear time. Research shows wounds heal faster when the wound bed is covered, keeping temperature consistent.
Is the wound dressing going to complement the type of wound?
Use dressings that conform to the wound and/or are easy to apply and remove. Heel wounds are a good example; you may need to design or select a heel cup type dressing to avoid bulkiness.
How much is the wound draining?
Use dressings that will keep the wound warm and that absorb the amount of drainage you have assessed. There are many longer wear time dressings available such as foams, super absorbents, and hydrocolloid dressings. Using a larger size of these dressing types will help protect the periwound as well.
What size of dressing should I use?
Protecting the periwound is as important as the wound. Prevent maceration to avoid further skin impairments by using a larger dressing containing superabsorbent polymers and that have moisture transfer and wicking properties will help protect the periwound area for the excess moisture. The use of skin protectants on the periwound will also help prevent maceration in patients at risk for moisture-associated skin damage (MASD).
Who is the payer source?
Unfortunately, we as clinicians need to follow dressing guidelines per payer source. Get familiar with the Medicare dressing guidelines because most payer sources follow this list. There may be certain insurances that require a preauthorization.
Who will be changing the dressing? Nurse or caregiver?
The patient and/or the caregiver(s) should be able to demonstrate the dressing application. Educate your patients and caregivers utilizing a teach-back method to ensure the patient and/or caregivers understand the dressing change procedure.
Other Considerations for Dressing Application
Once you have chosen the appropriate dressing, there are some other common dressing application specifics to look for or consider.
- Dressing compatibility: Does the use of viscous materials block the absorptive properties of the dressing? Do the properties of the dressing interfere with or deactivate collagenase or antimicrobial products?
- Ointment or cream thickness: Did you check for the correct dosage to ensure efficacy and prevent potential periwound maceration?
- Wear time of medicated dressing: Are you changing the dressing often enough to ensure consistent mechanism of action, wicking, or absorption?
- Cleanser compatibility: Is the dressing compatible with the cleansers you are using on the wound (to avoid cytotoxicity or deactivation of certain bioactive products)?
- Dressing size: If using a dressing larger than the wound, have you ensured that the periwound skin is protected from maceration? Can the dressing you chose be cut to fit the wound?
- Packing dead space: Have you ensured that the dressing will be entirely retrievable from the dead space (woven not to leave fibers, counting individual pieces, leaving a tail)?
- Clean wound bed: Have you ensured that any devitalized tissue that may block the mechanism of action of your dressing has been removed from the wound?1,2
Reimbursed Dressing Selection
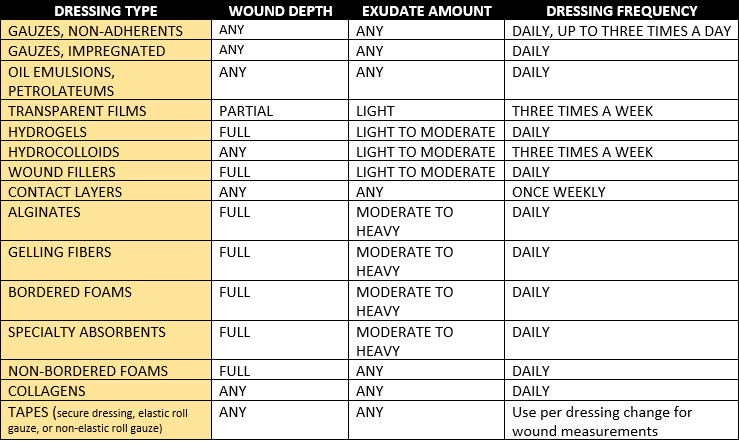
Wound care dressings, along with topical wound care agents, are driven by our Medicare guidelines payment system. Documentation of medical necessity for dressing reimbursement is vital. Wound assessment findings are used to justify dressing reimbursement in every setting. This includes wound date of onset, wound etiology, wound status, wound size, wound depth, presence of bioburden, drainage amount, dressing frequency, and wound progress notes as requested. Wound care clinicians should be familiar with payment systems per their health care setting because these systems may vary by health care setting and state region.4 As working health care clinicians, we should become familiar with dressing categories, indications, contraindications, and any warnings to help our patients in wound healing. Note: The information provided herein is for informational purposes. Always refer to manufacturer information for Indications, Warnings and Precautions for a specific product.
References
1. Carver C. WoundSource Blog: 8 Questions to Ask When Choosing a Wound Care Dressing. WoundSource.com. September 10th, 2015. Available at: http://www.woundsource.com/blog/8-questions-ask-when-choosing-wound-car…
2. Carver C. WoundSource Blog: The Future of Bioactive Wound Care Dressings WoundSource.com. April 12, 2016. Available at: http://www.woundsource.com/blog/future-bioactive-wound-care-dressings
3. PROPOSED/DRAFT Local Coverage Determination (LCD): Surgical Dressings (DL33831). Available at: https://www.cms.gov/medicare-coverage-database/details/lcd-details.aspx…;
4. Schaum KD. Medicare payment: surgical dressings and topical wound care products. Adv Wound Care (New Rochelle). 2014;3(8): 553–60. Doi. 10.1089/wound.2013.0434 PMCID: PMC4121050 PMID: 25126477 Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4121050/
The views and opinions expressed in this content are solely those of the contributor, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.










