Lower Extremity Wounds: Differential Assessment and Management
November 24, 2021
Determining Wound Etiology
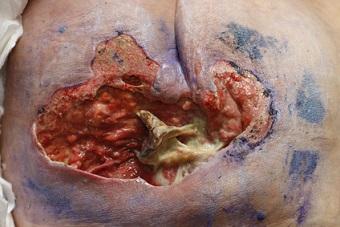
Predominant pain pattern, ulcer location, ulcer appearance, type and amount of wound exudate, and vascular and sensorimotor assessment are some key factors used to determine the primary etiology of lower extremity ulcers.1
Etiology Guides Treatment
Certain patients will have a clear presentation of wound etiology, whereas others may present with a mixed wound appearance. The certified wound specialist will complete a thorough history and physical assessment when determining wound etiology. From there, an individualized plan of care will be created, implemented, and continuously evaluated. For example1 :
- Venous ulcer: compression therapy and elevation
- Arterial ulcer: measures to improve tissue perfusion
- Neuropathic ulcer: offloading
In wounds of mixed etiology, the primary etiology should be addressed first, with modifications made to the plan of care based on additional findings. These modifications address the mixed etiology component. Patient education and follow-up, pain control, offloading, and behavioral and risk factor modification strategies, along with evidence-based topical therapies, are all important principles to incorporate into the plan of care.
Moist wound healing principles should be followed, along with infection prevention and control strategies when perfusion is confirmed. If there is a question related to ischemia, or suspected ischemia, and the wound is closed and uninfected, it should be kept clean, dry, and monitored for signs and symptoms of infection. Until perfusion is improved to a point that wound healing is supported, any ischemic ulcer should be kept clean, dry, and monitored for signs and symptoms of infection. Additionally, compression should be used with extreme caution in those with questionable arterial and neuropathic processes because the patient may be unable to detect sensory changes in the setting of increasing ischemia in the extremities.1
Interdisciplinary Approach and Referrals
When a comprehensive assessment is inconclusive or does not help in the determination of venous, arterial, neuropathic, or mixed disease, a referral may be needed. Additionally, in the setting of mixed disease when healing potential is unclear, when clinical signs of infection or osteomyelitis (probe to bone) are present, and when additional expertise may be required that may be beyond the scope or specialty of the referring provider, a referral should be initiated.
Some reasons for referral may include a request for total contact casting, tissue or bone biopsy, ordering customized footwear or compression garments, or a customized nutrition or pain management plan to promote healing and optimize quality of life. When management of the patient’s underlying comorbidities requires an interprofessional approach (examples: heart failure, peripheral vascular disease, diabetes, among others) to promote optimal wound healing, a referral should be initiated as well.1
Conclusion
As mentioned, lower extremity wounds can often be refractory or slow healing. These wounds require an interprofessional approach and effective, evidence-based management for optimal healing and prevention of recurrence. The first step in wound healing is to identify the cause. The causative and/or contributing factors must then be addressed for healing to occur.
A comprehensive assessment of vascular status, sensorimotor status, health history, pain pattern, location, and characteristics of the ulcer, as well as lifestyle modifications, should take place. This assessment, along with accurate understanding of the assessment data, is critical to positive patient outcomes. Treatment is then based on wound etiology, with modifications made to the plan of care in the setting of mixed disease. Referrals should be utilized as appropriate to promote healing and decrease future complications or refractory wounds.
Reference
1. McNichol L, Ratliff C, Yates S. Differential assessment of lower extremity wounds. In: McNichol LL, Ratliff CR, Yates SS, eds. Wound, Ostomy and Continence Nurses Society Core Curriculum: Wound Management. 2nd ed. Wolters Kluwer; 2022:446-453
About the Author
Holly is a Wound Care Coordinator at The Department of Veterans Affairs Medical Center in Cleveland, Ohio. She has a passion for education, teaching, and our Veterans. Holly has been practicing in wound care nursing for approximately six years. She has much experience with the long-term care population and chronic wounds as well as pressure injuries, diabetic ulcers, venous and arterial wounds, surgical wounds, radiation dermatitis, and wounds requiring advanced wound therapy for healing. Holly enjoys teaching new nurses about wound care and most importantly, pressure injury prevention. She enjoys working with each patient to come up with an individualized plan of care based on their needs and overall medical situation. She values the importance of taking an inter-professional approach with wound care and prevention overall, and involves each member of the healthcare team as much as possible. She also values the significance of the support of leadership within her facility and the overall impact of great teamwork for positive outcomes.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.










Follow WoundSource
Tweets by WoundSource