Benefits of a Portable, Mechanical Negative Pressure Device for Pediatric Patients
December 9, 2022
Introduction
The benefit of Negative Pressure Wound Therapy (NPWT) as an “active,” adjunctive treatment is well-established. Evidence has shown that wounds treated with negative pressure granulate faster than wounds managed with traditional dressings. There is ever-increasing literature to support the use of NPWT to treat wounds effectively and safely in even the youngest patients.1 Some specific benefits of NPWT for pediatric and adolescent patients include decreased frequency of dressing changes, as well as a dressing that is occlusive and unlikely to be removed by the patient.
Pediatric Considerations for NPWT Use
NPWT should be used cautiously in pediatric patients to prevent complications. There are several factors to consider when using NPWT to treat a pediatric patient. These factors may vary based on the age and developmental level of the child and include the following1-3:
- Many recommendations support using a lower level of negative pressure in small infants and gradually increasing negative pressure in older infants and toddlers. The level of negative pressure applied to the wound bed should be set near or below the mean arterial pressure (MAP) in very young patients.
- Large areas of skin are often covered with clear adhesive film when an NPWT dressing is applied. Immature skin structure should be considered when applying and removing adhesives from the skin. Silicone-based, alcohol-free skin barrier films should be applied under the adhesive drape to prevent skin stripping and adhesive trauma. Silicone-based adhesive removal products may be used further to prevent medical adhesive-related skin injury (MARSI). NPWT drapes with silicone adhesive may be particularly beneficial for pediatric patients.
- Periwound skin should be protected from negative pressure with a layer of transparent adhesive film or a thin hydrocolloid.
- NPWT dressing changes may be longer or more involved than a standard wound dressing change. It may be beneficial to involve a parent or Child Life Specialist to engage or distract the child during NPWT dressing changes. NPWT dressing changes on larger, more complex wounds may require a trip to the operating room.
- To minimize pain and bleeding during dressing changes, a nonadherent mesh contact layer may be placed under the foam in the wound bed. Topical lidocaine applied directly to the wound bed has also been shown to be beneficial.
- Use of continuous, rather than intermittent NPWT, is recommended for pediatric patients, as the intermittent setting may be startling or cause increased pain.
Limitations of Traditional NPWT in Pediatrics
Traditional NPWT uses electrical or battery power to generate negative pressure. The NPWT pump must remain plugged into an outlet. When unplugged, the pump's battery life is often limited to 6 hours or less. These factors may limit the mobility and activity of an otherwise active child. Clinicians should take note of the following when assessing the usefulness of traditional NPWT in pediatric patients:
- Portable versions of electrically powered NPWT devices are often too heavy or cumbersome for a mobile toddler or young child to carry.
- If a child is able to carry the portable NPWT pump, they are still limited by the need to connect to an electrical outlet.
Electrically powered NPWT may be best suited for inpatient use in pediatric patients due to these limitations listed above. Mechanical NPWT is often a better fit for pediatric patients.
Benefits of Mechanical NPWT in Pediatric Patients
Mechanical NPWT devices use a spring and coil mechanism to generate negative pressure. These devices offer numerous benefits for pediatric patients and open the door for the use of NPWT in the outpatient pediatric population, including the following:
- The patient is not restricted by their connection to a heavy NPWT pump.
- No electrical outlet or battery is required.
- The small, lightweight canister is easily portable, even for the smallest crawlers or walkers. The canister is about the size of a cell phone.
- The canister may be worn on a strap around the patient’s body or extremity.
- The mechanical NPWT system is completely silent compared to a traditional electric pump, which makes noises that may be startling for young children.
To further illustrate the effectiveness of mechanical NPWT use in the pediatric population, please consider the following case study.
Case Study
I was consulted to evaluate a wound on an active 18-month-old patient with Hemophagocytic lymphohistiocytosis (HLH). This patient had necrosis at the site of an implanted port on her upper chest. The port was surgically removed, and the incision subsequently dehisced. The wound was left to heal by secondary intention. This patient needed a bone marrow transplant for treatment of her HLH. She could not be considered for the procedure with her open wound. Initially, traditional wound dressings were selected, which followed the principles of moist wound healing. As the wound failed to show adequate progress after a couple of weeks, more advanced dressings were selected, but the wound remained recalcitrant. Neutropenia and chemotherapy were suspected to be contributory factors.
The depth of the wound and clean wound bed made it ideal for the use of a more aggressive therapy like NPWT. However, this patient only received treatment twice a week at clinic appointments, a frequency not amenable for the use of a cumbersome electrical NPWT device. After 42 days of using standard wound dressings, a mechanical NPWT system was placed. The canister was worn via a soft strap around the patient’s trunk. The dressing was changed twice a week during clinic visits for a period of 42 days and was performed without any analgesic medications. Silicone-based skin barrier film and adhesive removal spray were used with each dressing change. The wound showed significant progress at the time of the first NPWT dressing change and with each subsequent change. After discontinuation of NPWT, an antimicrobial foam dressing containing methylene blue and gentian violet was used to support continued healing.
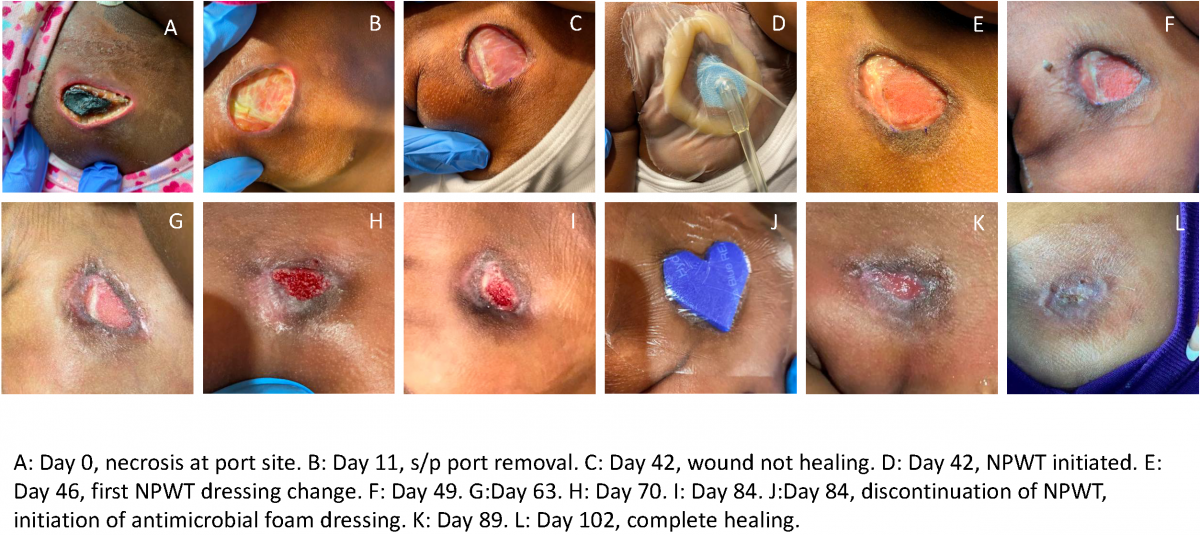
Figure 1
By day 102, the wound achieved complete healing, as shown in the figure above in image "L." The mechanical NPWT device was ideal for this patient and offered a unique solution for her nonhealing wound.
Conclusion
For the pediatric patient population with nonhealing wounds, mechanical NPWT can prove to be an effective adjunctive treatment. Every device and adjunctive therapy has its strengths and weaknesses depending on the patient’s individual circumstances, the wound’s level of severity, and other factors. When assessing a pediatric patient with a recalcitrant wound, mechanical NPWT may be the lightweight treatment that facilitates the best outcome.
References
- Lund C, Singh C. Skin and Wound Care for Neonatal and Pediatric Populations. In: Doughty DB, McNichol LL, editors. Wound, Ostomy and Continence Nurses Society Core Curriculum Wound Management. Philadelphia, Wolters Kluwer; 2016. 198-219.
- Agrawal V, Wilson K, Reyna R, Emran MA. Feasibility of 4% Topical Lidocaine for Pain Management During Negative Pressure Wound Therapy Dressing Changes in Pediatric Patients: A Case Study. J Wound Ostomy Continence Nurs. 2015 Nov-Dec;42(6):640-2.
- Dechant ED. Considerations for Skin and Wound Care in Pediatric Patients. Phys Med Rehabil Clin N Am. 2022 Nov;33(4):759-771.
About the Author
Elizabeth Day Dechant, BSN, RN, CWOCN, CFCN is a Certified Wound Ostomy Continence Nurse at Children’s of Alabama, where she provides wound treatment recommendations and wound management for both inpatients and outpatients with acute and chronic wounds. She provides staff education on skin and wound care, ostomy care, and pressure injury prevention. Elizabeth works diligently with the hospital’s Pressure Injury Prevention Team to track and reduce hospital-acquired pressure injuries.
The views and opinions expressed in this content are solely those of the contributor, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.










